I’ve been struggling to write a “Dear Doctors” post for a while. Everything that I’ve tried to write has been too bitter, or too manic, or too scolding, and nothing has yet been published.
I recently stumbled across a great article though, and I now have a “Dear Doctors” letter. Here it is:
Dear Doctors,
Read this:
Journal of Investigative Medicine HIGH IMPACT CASE REPORTS, “Permanent Peripheral Neuropathy: A Case Report on a Rare but Serious Debilitating Side-Effect of Fluoroquinolone Administration“
And please change how you prescribe fluoroquinolones accordingly.
Thank you,
Lisa Bloomquist
The article is great and I highly recommend that everyone read it. Following is my breakdown of it. Everything that is italicized is a direct quote from “Permanent Peripheral Neuropathy, A Case Report on a Rare but Serious Debilitating Side-Effect of Fluoroquinolone Administration” by Dr. Jacquelyn K. Francis and Dr. Elizabeth Higgins. (Everything that is not italicized is my commentary.) The article was published in the Journal of Investigative Medicine High Impact Case Reports and was published on July 27, 2014.
INTRO
While there has been success in recent years in decreasing the numbers of unnecessary antibiotic administrations, still rampant in medical practice is the inappropriate use of antibiotics. Fluoroquinolones administration is no different.
Indeed – fluoroquinolones are being prescribed inappropriately. Not many people are arguing that fluoroquinolone antibiotics should be banned. Most of us are arguing that fluoroquinolone antibiotics are used INAPPROPRIATELY, and in being used inappropriately they are causing unnecessary harm.
These bactericidal agents are capable of central nervous system (CNS) penetration, with an impressive treatment profile that includes an enhanced spectrum of activity, high oral bioavailability, high serum drug concentration that parallels that of intravenous drug administration, and rapid mechanism of action. It is for this reason that physicians favor these drugs for treatment of simple infections, which range from uncomplicated urinary tract infections (UTIs) and gastrointestinal infections to lower respiratory infections and pneumonias.
Unfortunately, they’re not APPROPRIATE for use in treating simple infections. Fluoroquinolones are strong drugs. They are chemotherapy drugs masquerading as antibiotics. But doctors reach for them for simple infections because, well, these two quotes illustrate the problem well:
In The New York Times article, “Popular Antibiotics May Carry Serious Side-Effects” it was noted that, “In an interview, Mahyar Etminan, a pharmacological epidemiologist at the University of British Columbia, said the drugs were overused ‘by lazy doctors who are trying to kill a fly with an automatic weapon.’”
In “Your Doctor’s Knee-Jerk Reflex: How Not to Get Kicked” by Dr. David Katz, M.D., published in the Huffington Post, it was noted that, “Often, the easiest way for a busy clinician to be sure to ‘cover the bases’ with an antibiotic is to go after a fly with an elephant gun. The collateral damage can, predictably, be considerable; a consequence of knee-jerk prescribing.”
According to established guidelines, however, these antibiotics are recommended as drugs of last resort and for treatment of cases refractory to other safer antibiotic alternatives.
When it is uncovered that the increase in rates of fibromyalgia, autism, autoimmune diseases, diabetes, chronic fatigue syndrome / M.E., ALS, Alzheimer’s Disease, Lymphoma and other diseases since 1990 is due to fluoroquinolones, doctors will cry to the FDA and AMA about how they weren’t warned. But they were warned. FDA and AMA guidelines state that fluoroquinolones should only be used as a last resort and that magnesium levels should be checked prior to administration of fluoroquinolones. Too many doctors just ignored those recommendations.
Reports in recent years of the adverse drug events of these drugs are on the rise, with not only an overrepresentation of common antibiotic complaints, including diarrhea, nausea, and headache that occur at rates higher than most other antimicrobials on the market, but there is also mounting evidence suggesting the potential for long-term adverse peripheral nervous system (PNS) effects from fluoroquinolone usage. The need for physicians to be judicious when prescribing these drugs is therefore paramount.
Patients are crossing their tolerance thresholds for fluoroquinolones. There is only so much damage that their cells can withstand, and people are developing fluoroquinolone toxicity syndrome after crossing their cellular damage threshold.
Yes, physicians need to be judicious when prescribing these drugs. That would be lovely.
CASE PRESENTATION
A 57-year-old Caucasian female presented to outpatient clinic with complaints of dysuria, polyuria, and urinary urgency. Urinalysis showed 2+ leukocytes and trace blood. Based on her clinical presentation, she was treated for UTI with a ciprofloxacin regimen of 250 mg twice a day for 5 days. Subsequent urine culture showed no evidence of organism, and against advice for reevaluation, she was lost to follow-up. She presented 2 months later reporting whole body burning and alopecia. The burning, she claimed, started 2 or 3 days after completion of the prescribed course of ciprofloxacin. The burning lasted 3 weeks and resolved only to recur, unrelentingly, 3 weeks later. She had been unable to adorn clothing during this time, for she said this triggered whole body burning. At the point wherein she was finally able to wear clothing, she presented to the clinic. Hydration and Epsom salt soaks provided no relief. She reported pain of 10/10.
Note that the patient DIDN’T EVEN HAVE AN INFECTION. She was poisoned with ciprofloxacin when there wasn’t even an infection. Talk about INAPPROPRIATE! Criminal is more like it!
Her peripheral neuropathy pain was so bad that she was “unable to adorn clothing during this time, for she said this triggered whole body burning.” THAT. IS. HORRIBLE! A pain level of 10/10 is what she experienced. That is a SEVERE adverse reaction and even the possibility of a reaction like that should dissuade doctors from prescribing fluoroquinolones frivolously.
She didn’t even have an infection. It boggles my mind.
Her past medical history is significant for trigeminal neuralgia, in remission for 12 years. The patient was on no medications at the time of her visit. She has no specific medication allergies, but does get gastrointestinal symptoms with opioids, namely, fentanyl. Physical examination was unremarkable. Vitals at the time that she was seen included the following: blood pressure 132/78 mm Hg, temperature of 97°F, heart rate of 60 beats per minute, respirations of 18. Her body mass index was 17.94, down from 20.3 two months earlier. On detailed neurologic examination, cranial nerves II through XII were intact bilaterally. There was no pronator drift of outstretched arms. There was some muscle wasting in biceps; however, overall tone was normal. Strength was full bilaterally. Reflexes were 2+ and symmetric at the biceps, triceps, knees, and ankles. Plantar responses were flexor. Light touch and pinprick produced pain and paresthesias diffusely in the upper and lower extremities; however, position sense and vibration sense were intact in fingers and toes. Rapid alternating movements and fine finger movements were intact. There was no dysmetria on finger-to-nose and heel-knee-shin. There were no abnormal or extraneous movements. Romberg was absent. The patient’s posture was normal. Gait was steady with normal, though tentative, steps, base, arm swing, and turning. Heel and toe walking were normal. Tandem gait was normal. She had no discernable rash or skin lesions.
Subsequent complete blood work analysis to check for an electrolyte abnormality basis of her complaints was unremarkable. Her complete blood count was normal with a hematocrit of 41%. Her vitamin B12 level was 258 pg/mL, with a normal range of 200 to 900 pg/mL. Her thyroid stimulating hormone level was 2.05, with a normal range of 0.4 to 6.0. Her immunoglobulin levels were normal. Her vitamin D level was 13 nmol/L (optimal >30 nmol/L). Copper level was 98 mg (normal 50-80 mg). Vitamin E was normal at 12.7 µg/mL (normal range = 5.5-17 µg/mL). Vitamin B1 was normal at 5.4 µg/dL (normal range = 2.5-7.5 µg/dL).
Her blood work and further questioning could provide no new medical etiology for her symptoms, and so the patient was subsequently sent for complete neurological workup. Workup included heavy metal toxicity screening to assess for possible heavy metal exposure to lead, mercury, cadmium, and zinc. Electrophysiological studies were also done to assess neuromuscular nerve action potential transmission, a test that could discern a neuromuscular disorder etiology. Three-millimeter skin punch biopsy to assess for small fiber density and possible neurologic process were also done. These tests were all negative. Neurological workup could not determine a unique cause of her symptoms. It was concluded that if her symptoms were neurologic-based, it was, in fact, a multifocal process.
Fluoroquinolone toxicity syndrome has been unrecognized for so long for many reasons. One of the biggest reasons is that the tests all come out “normal.” This simply means that the tests are wrong. If a patient has pain levels that are a 10/10, there’s something wrong with her and if the tests don’t show it, the tests aren’t sufficient.
Two years after the initial onset of symptoms, the patient continues to suffer from polyneuropathies chronologically related to ciprofloxacin use. At her most recent visit, she describes constant pain of 7/10 and is unable, she states, to ambulate for more than 2 minutes, without intense shooting pains up and down her lower extremities. She describes “pins and needles” up and down her legs and thighs radiating to her buttocks and feet. She claims that her upper body and abdomen have now been spared of such feelings. She describes severe alopecia and ambulates now with a broad-based gait. She describes being on permanent disability because of her condition. The rest of her physical examination remains unchanged. There are no gross neurological deficits discernible on neurologic examination. The patient remains on amitriptyline 20 mg daily for control of her pain symptoms.
This patient’s life has been ruined. My heart goes out to her. Two years later, she still suffers from chronic pain and is now disabled. THIS IS NOT OKAY.
DISCUSSION
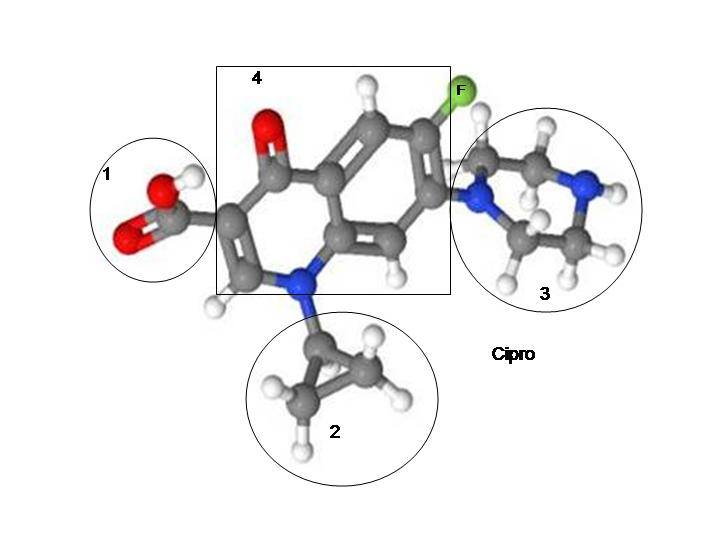
Fluoroquinolones are fluorinated quinolones, the only bactericidal agent in the antibiotic class capable of directly inhibiting DNA synthesis.
Fluoroquinlones may not be the only antibiotics that damage mitochondria, but they are the only antibiotic class that inhibits DNA synthesis. And who, exactly, thought it would be a good idea to give people drugs that inhibit DNA synthesis?
The harm that fluoroquinolones do to DNA shouldn’t come as a surprise. It was noted in “Quinolone binding to DNA is mediated by magnesium ions” in 1992 that, “Even if reconsidered in terms of affinity, the interaction with DNA is still of great concern because of the possible long-term genotoxicity of quinolone compounds, which are increasingly adopted as first-choice antibiotics for the treatment of many infections, and because it addresses the real mechanism of action for this class of molecules.”
Caution was warranted. It was not used.
They do this by promoting cleavage of bacterial DNA in the DNA–enzyme complexes of DNA gyrase and topoisomerase IV. Generally, gram-negative antibacterial activity correlates with inhibition of DNA gyrase, and gram-positive antibacterial activity corresponds with inhibition of DNA type IV topoisomerase. With the introduction of these drugs in the 1960s, physicians were able, for the first time, to treat severe gram-negative infections orally. The first successful fluorination of part of the quinolone drug in 1986, in the form of norfloxacin, brought with it the capability of crossing the blood–brain barrier and achieving CNS penetration.
Fluoroquinolones have the capacity to cross the blood-brain barrier and achieve CNS penetration. NOT GOOD.
This and the already great treatment profile in the form of enhanced spectrum of activity, high oral bioavailability, high serum drug concentration comparable to intravenous infusion, and rapid mechanism of action added to the popularity of these drugs ultimately resulting in the indiscriminate use of these drugs. The enhanced treatment profile of these drugs came at a price however, with adverse effects so severe that use of many fluoroquinolones since then being restricted or the drugs withdrawn from the market entirely.
These drugs have been used indiscriminately at a huge price. If, as I suggested above, the increase in chronic, debilitating, mysterious diseases that has come about since 1990 is, indeed, due to fluoroquinolones, the “price” of these drugs is even greater than what the study’s authors have noted.
One of the challenges of diagnosing a patient with fluoroquinolone-associated peripheral neuropathy is the diffuse, confusing, and delayed array of symptoms that can occur. A 1996 study first brought these adverse effects to light.
I could cry. Delayed adverse reactions are noted in a journal article. The fact that symptoms are diffuse, confusing, and difficult to diagnose is acknowledged in a journal article. E-hugs to Dr. Francis and Dr. Higgins.
While patients on the fluorinated drugs exhibited less side effects than those associated with first-generation quinolone predecessors, such as nausea and gastrointestinal disturbances, 0.9% to 1.6% experienced adverse reactions relating to the peripheral and central nervous system, including headache, dizziness, drowsiness, agitation, psychosis, and convulsions, as well as peripheral sensory disturbances, symptoms that had never been complained of prior, at least not on any significant scale.
It is not okay to induce possibly permanent nervous system damage in .9 to 1.6% of those who take fluoroquinolones – especially when the nervous system damage can be permanent. 26.9 million prescriptions for fluoroquinolones were written in 2011 alone. .9% of 26.9 million is 242,100 and 1.6% of 26.9 million is 430,400 – PEOPLE. Between 242,100 and 430,400 people had adverse central and/or peripheral nervous system side-effects.
Note that peripheral nervous system damage from fluoroquinolones could easily be mistaken/misdiagnosed as fibromyalgia, and central nervous system damage can lead to depression, anxiety and other psychiatric illnesses.
Of these patients, 81% had symptoms occurring within 1 week of drug administration, with paresthesia being the mainly reported symptom. Five years later, a 2001 study found that contrary to previous reports suggesting that fluoroquinolone-associated PNS events are mild and short term, 80% of study participants reported severe events that typically involved multiple organ systems, especially the PNS, with symptom onset as early as 24 hours within initiation of treatment. 58% of these cases had symptoms lasting greater than 1 year.
Indeed. My thanks to the authors of this paper for noting that peripheral nervous system adverse reactions to fluoroquinolones are neither mild nor short term. Compared to other floxies, my reaction was moderate – and I still had pain for more than a year.
Another 2001 formal study that sought to assess the prevalence of fluoroquinolone-induced PNS adverse side effects highlighted the severity of these effects. The study concluded that there was a high association between fluoroquinolone antibiotics and severe, long-term adverse PNS and multiple organ system effects that included PNS sensory symptoms (91%), peripheral neuropathy motor symptoms (55%), and CNS effects (75%). Over 80% of the patients surveyed had sequalae stemming from fluoroquinolone use that lasted for greater than 1 year. A subset of these patients and their adverse drug events are included in Table 1.
Risk is a function of frequency and severity of adverse reactions. Adverse reactions to fluoroquinolones are severe. I don’t think that they’re rare (https://floxiehope.com/2013/08/09/is-fluoroquinolone-toxicity-rare/). Fluoroquinolones are far too risky to be used as they are currently being used.
Despite these seemingly significant numbers and overwhelming reports from patients, physicians continue to prescribe fluoroquinolone antibiotics unsystematically, against US Food and Drug Administration recommendations. The pressures of health care facilities and patients alike to increase patient turnaround and quickly alleviate symptoms may compound this problem.
Dear doctors – please, please, please listen. Please listen to your patients, listen to the AMA and the FDA, and listen to your colleagues who wrote this case-study. We see that fluoroquinolones are dangerous drugs and we are trying to tell you about them.
As highlighted in the aforementioned case, the peripheral neuropathy reported with fluoroquinolone administration can be severe, debilitating, and permanent. It is for this reason that physicians need to practice due diligence when prescribing not only antibiotics, but any drug.
THANK YOU Dr. Francis and Dr. Higgins!
Physicians also need to practice vigilance in the event of an adverse reaction. They can do this with careful follow-up of patients and ensure that patients are aware of all the side effects that may be associated with their prescribed drug. Patients need to know what to look for and where to go in the event that one of these symptoms become manifest. It is our hope that the updated FDA warning and presentation of this case will encourage physicians to be more conscientious of their treatment selections.
Yes, we need recognition and an appropriate treatment protocol for everyone suffering from fluoroquinolone toxicity. Thank you for saying it so well, Drs. Francis and Higgins!
TAKE HOME POINTS
- The FDA recommends that fluoroquinolones be used as a drug of last resort and for treatment of cases refractory to other safer antibiotic alternatives.
- The FDA updated their black box warnings on all fluoroquinolones to stress the rapidity of onset and permanence of peripheral neuropathy associated with their use.
- Physicians should be aware of the risks and side effects associated with the drugs that are prescribed and be able to inform patients of the risks associated with the use of these drugs.
- Physicians should always aim to administer the least broad spectrum antibiotic possible based on known sensitivities and regional resistance PATTERNS.
I know that I’m incredibly biased, but I think that the tide is shifting. I think that the severity of adverse reactions to fluoroquinolones are being recognized. With recognition will come change in their behavior.
I hope for change.










… [Trackback]
[…] Read More Information here to that Topic: floxiehope.com/peripheral-neuropathy-case-fluoroquinolone/ […]
… [Trackback]
[…] Read More here to that Topic: floxiehope.com/peripheral-neuropathy-case-fluoroquinolone/ […]
… [Trackback]
[…] Find More to that Topic: floxiehope.com/peripheral-neuropathy-case-fluoroquinolone/ […]
… [Trackback]
[…] There you can find 51006 additional Information on that Topic: floxiehope.com/peripheral-neuropathy-case-fluoroquinolone/ […]
… [Trackback]
[…] Read More here on that Topic: floxiehope.com/peripheral-neuropathy-case-fluoroquinolone/ […]
… [Trackback]
[…] There you can find 14407 additional Info to that Topic: floxiehope.com/peripheral-neuropathy-case-fluoroquinolone/ […]
… [Trackback]
[…] Find More here to that Topic: floxiehope.com/peripheral-neuropathy-case-fluoroquinolone/ […]
… [Trackback]
[…] Read More to that Topic: floxiehope.com/peripheral-neuropathy-case-fluoroquinolone/ […]
… [Trackback]
[…] Find More on to that Topic: floxiehope.com/peripheral-neuropathy-case-fluoroquinolone/ […]
… [Trackback]
[…] There you can find 76384 additional Info to that Topic: floxiehope.com/peripheral-neuropathy-case-fluoroquinolone/ […]
… [Trackback]
[…] Find More on to that Topic: floxiehope.com/peripheral-neuropathy-case-fluoroquinolone/ […]
… [Trackback]
[…] Here you will find 63650 more Info to that Topic: floxiehope.com/peripheral-neuropathy-case-fluoroquinolone/ […]
… [Trackback]
[…] Info on that Topic: floxiehope.com/peripheral-neuropathy-case-fluoroquinolone/ […]
… [Trackback]
[…] Find More to that Topic: floxiehope.com/peripheral-neuropathy-case-fluoroquinolone/ […]
… [Trackback]
[…] Find More here to that Topic: floxiehope.com/peripheral-neuropathy-case-fluoroquinolone/ […]
… [Trackback]
[…] Find More Info here on that Topic: floxiehope.com/peripheral-neuropathy-case-fluoroquinolone/ […]