The post, Do Fluoroquinolone Antibiotics Trigger Charcot-Marie-Tooth and Other Genetic Diseases?, was published on Hormones Matter today (3/7/16).
I hope that you find the connections to be interesting, and not too frightening.
A couple things to note: First, Charcot-Marie-Tooth disease has nothing to do with teeth – Dr. Tooth was one of the people who discovered and named it. Second, though there are potential connections between fluoroquinolone toxicity and several genetic diseases, this is just a hypothesis, so please take it as just that. The connections are interesting, and should be explored. However, I don’t want anyone reading this, or anything else I write, to think that you are doomed.
Many “floxies” have expressed that they feel as if they have aged 20 years in a matter of weeks or months. I wonder if, on a cellular level, they actually have. I wonder if fluoroquinolones age cells and, in doing so, trigger diseases that would have remained dormant until much later in life. I wonder how fluoroquinolones, and other pharmaceuticals, affect gene expression (epigenetics), and if those effects are passed down from one generation to the next. I honestly don’t know the answer to these questions.
IF the damage mechanism for fluoroquinolones is genetic damage, and underlying diseases are triggered, reactions would be different for each person. This could explain the huge variation in fluoroquinolone toxicity reactions. Unfortunately, if this is the case, I think that we’re a long way from proving connections between fluoroquinolones and the triggering of diseases that are thought to be genetic in nature. Epigenetics is a relatively new area of study, and the triggering of epigenetic changes via pharmaceuticals isn’t something that I’ve run across much in my research. I think that it’s a topic that deserves significantly more attention.
Please read and share “Do Fluoroquinolone Antibiotics Trigger Charcot-Marie-Tooth and Other Genetic Diseases?” Thank you!
_____________________________________________________________________________
The following fascinating article was published under a Creative Commons License, meaning that it can be published freely. It was originally published on www.mosaicscience.com – a great site that I highly recommend you check out. The article is about uncovering some of the genes behind Charcot-Marie-Tooth Disease. It’s also about being your own biggest advocate, and pushing to solve health “mysteries.”
DIY diagnosis: how an extreme athlete uncovered her genetic flaw
Kim Goodsell was running along a mountain trail when her left ankle began turning inward, unbidden. A few weeks later she started having trouble lifting her feet properly near the end of her runs, and her toes would scuff the ground. Her back started to ache, and then her joints too.
This was in 2002, and Kim, then 44 years old, was already an accomplished endurance athlete. She cycled, ran, climbed and skied through the Rockies for hours every day, and was a veteran of Ironman triathlons. She’d always been the strong one in her family. When she was four, she would let her teenage uncles stand on her stomach as a party trick. In high school, she was an accomplished gymnast and an ardent cyclist. By college, she was running the equivalent of a half marathon on most days. It wasn’t that she was much of a competitor, exactly – passing someone in a race felt more deflating than energising. Mostly Kim just wanted to be moving.
So when her limbs started glitching, she did what high-level athletes do, what she had always done: she pushed through. But in the summer of 2010, years of gradually worsening symptoms gave way to weeks of spectacular collapse. Kim was about to head to Lake Superior with her husband, CB. They planned to camp, kayak, and disappear from the world for as long as they could catch enough fish to eat. But in the days before their scheduled departure, she could not grip a pen or a fork, much less a paddle. Kim, a woman for whom extreme sports were everyday pursuits, could no longer cope with everyday pursuits. Instead of a lakeside tent, she found herself at the Mayo Clinic in Rochester, Minnesota.
After four days of tests, Kim’s neurologist told her that she had Charcot–Marie–Tooth disease, a genetic disorder that affects the peripheral neurons carrying signals between the spinal cord and the extremities. It’s rare and carries a varying suite of symptoms, but Kim’s are typical, starting at the feet and heading upward. The neurologist explained that as her neurons died, the surviving cells picked up the slack by sprouting new branches – a workaround that masked the underlying degeneration until the rate of cell death outpaced the rate of compensation. Hence Kim’s crash.
The neurologist told her to come back in a year so he could check how quickly the disease was progressing, but that it would certainly progress. Charcot–Marie–Tooth has no cure.
The Goodsells drove home and Kim, exhausted, slept for two days. When she woke up, she got to work. “My reaction to things that I have no control over is to find out as much as I can about them,” she says. She started by reviewing her clinic notes, and quickly noticed something odd: there was hardly any mention of her heart.
Years before she learned that she had Charcot–Marie–Tooth, Kim discovered that she had another genetic disorder – one that affects the heart, arrhythmogenic right ventricular cardiomyopathy (ARVC). ARVC gradually replaces the heart’s synchronised beating muscle with fat and scar tissue. It nearly killed her once; she still has an internal defibrillator to keep her heart beating. But even though it was there in her medical records, her neurologist hadn’t seen fit to mention it in his report. “It meant nothing to him,” says Kim. “I thought: Wow, that’s really funny.”
It wasn’t the omission per se that bothered her. It was the implicit suggestion that her two life-long diseases – one of the heart, one of the nervous system – were unrelated. That, in the genetic lottery, she was a double-loser. That lightning must have struck her twice.
Surely not, she thought. Surely there must be a connection.
I meet Kim at La Ventana in Baja California, Mexico. She spends winters here, mostly kitesurfing. The sand and water are postcard-quality, but La Ventana has barely any resorts or big hotels. So in the still air of the morning when kites won’t fly, the beach is empty. Kim likes it that way. She has been up since dawn, cycling among the cacti and swimming in the ocean with pelicans and frigatebirds for company. She hauls herself out of the water, dries off, and sits on a small terrace overlooking the ocean. Her face is tanned and wrinkled, and she manifests no obvious signs of her two conditions. That’s partly because she has developed workarounds to mask and control her symptoms. She brushes her teeth on one foot to offset her balance problems. She uses massage balls and spends hours stretching to stop her muscles and joints from seizing up.
“See how I’m sitting?” she says. She has pulled her legs up on the chair to her left, and her back is curving that way too.
“My spine curves this way” – she nods to the right – “so I sit curving to the opposite side. I consciously do the opposite.”
She has a history of that. In 1979 Kim was a mathematically gifted pre-med student at UC San Diego, her hometown college. Her path was clear: graduate, and follow her older brother into medical school. But on a trip to South America – her first time out of San Diego – she ended up hiking for three months instead of working at a clinic as she’d planned. When she returned home, her academic future seemed pale and uninspiring. And then CB – her future husband, at this point a fellow student and regular running partner – started taking her out on wilderness hikes. “He introduced me to the mountains and I thought: this is life,” Kim says.
Within months of graduating Kim dropped out. Her brother, who had been a father figure to her growing up, was furious. “We hardly spoke. CB was his friend and he couldn’t even look at him,” she says. “He said I was being completely irresponsible.” Kim and CB married in 1983, and aside from a brief stint as restaurant owners, they have never had 9-to-5 jobs. They mostly earned a living by buying and remodelling run-down houses and selling them at a profit, and then heading into the wilderness until their supplies ran out. In 1995 they found themselves in La Jolla, California, working on an especially stressful renovation that left Kim drained.
That was when her heart problems began. Kim started having episodes of ventricular tachycardia – the lower chambers of her heart contracted so quickly that they pumped out their contents before they had a chance to fill up, compromising the flow of blood (and therefore oxygen) to the rest of her body. One minute she would be racing down Highway 1 on her bike; the next she would feel like she had been “unplugged”, as if “there was nothing driving anymore”. A cardiologist at Scripps Memorial Hospital told her she’d need an internal defibrillator, but Kim said no – she was worried it’d get in the way of wearing a backpack on a run, and she had faith that she’d be able to deal with the ventricular tachycardia by slowing down and relaxing. “I didn’t want something implanted in me that would limit my opportunities of experiencing life,” she says.
The next week, the Goodsells finished their renovation, packed up and headed into the Sierra Nevada with no return date in sight. It was an unorthodox solution to a life-threatening heart condition: to vanish into the boondocks, far away from any medical care, to do even more exercise.
The thing is, it was the right one. The outdoors rejuvenated her. She was gone for one-and-a-half years, and her heart behaved the whole way through. That unbroken streak only broke when the Goodsells rejoined their old lives in 1997. Back in California, they were once again cycling down Highway 1 when her heart started to beat erratically again. This time, it did not stop.
By the time the paramedics arrived, Kim was slumped against a wall and her chest was shaking. Her tachycardia had lasted for almost an hour and progressed to ventricular fibrillation – that is, her heartbeat was erratic as well as fast. She blacked out in the ambulance, on the cusp of cardiac arrest.
She woke up at Scripps Memorial Hospital. The same cardiologist was there to greet her. Through further tests he discovered that the muscle of her right ventricle was marbled with fat and scar tissue and not contracting properly. These are classic signs of ARVC. It had only been properly described in 1982, back when Kim was regularly signing up for triathlons. ARVC is a major cause of fatal heart attacks in young people, and athletes are especially vulnerable as exercise can accelerate the disease’s progress. And since Kim wouldn’t stop exercising, she finally conceded to the defibrillator. They implanted it the next day.
Kim referred to the implant as her “internal terrorist”. Every shock was debilitating and led to months of anxiety. She had to learn to cope with the device, and it took several years to regain the joy she drew from hardcore exercise. That was when the other symptoms started.
These diseases are rare. In a crowd of a million adults, around 400 will have Charcot–Marie–Tooth and between 200 and 400 will have ARVC. But genetic diseases in general are actually quite common – 8 per cent of people have at least one. This paradoxical combination has fuelled the rise of many online communities where people with rare disorders can find each other. Heidi Rehm, a geneticist at Harvard Medical School, studies a condition called Norrie disease that mostly affects the eyes and ears. She developed a registry for Norrie disease patients to share their experiences, and learned that almost all the men with the disease had erectile dysfunction. “A patient goes to their doctor with blindness and deafness, and erectile dysfunction isn’t the first thing you ask about!” says Rehm. “Patients drove that discovery.” Through communities, families often make connections about their medical problems that their doctors miss.
But Kim was never one for relying on others. She tried a support group when she got her implant, but it did nothing for her. She dipped her toes in patient forums, but was always frustrated by the rampant misinformation. “People just weren’t interpreting things correctly,” Kim says. “I wanted more rigour.”
She started by diving into PubMed – an online search engine for biomedical papers – hunting down everything she could on Charcot–Marie–Tooth. She hoped that her brief fling with a scientific education would carry her through. But with pre-med knowledge that had been gathering dust for 30 years and no formal training in genetics, Kim quickly ran headfirst into a wall of unfamiliar concepts and impenetrable jargon. “It was like reading Chinese,” she says.
But she persisted. She scratched around in Google until she found uploaded PDFs of the articles she wanted. She would read an abstract and Google every word she didn’t understand. When those searches snowballed into even more jargon, she’d Google that too. The expanding tree of gibberish seemed infinite – apoptosis, phenotypic, desmosome – until, one day, it wasn’t. “You get a feeling for what’s being said,” Kim says. “Pretty soon you start to learn the language.”
“Kim has an incredible ability to understand the genetic literature,” says Martha Grogan, a cardiologist from the Mayo Clinic and an old friend of CB’s who now coordinates Kim’s care. “We have a lot of patients who ask great questions but with Kim, it’s like having another research fellow.”
At the time the Goodsells were staying at a friend’s house at Lake Michigan. Kim would sit on the balcony for eight hours a day, listening to the water and teaching herself genetics. Too weak to explore winding hillside trails, she channelled her perseverance and love of isolation towards scientific frontiers and the spiralling helices of her own DNA. “I spent hundreds of hours,” she says. “CB lost me during this process.”
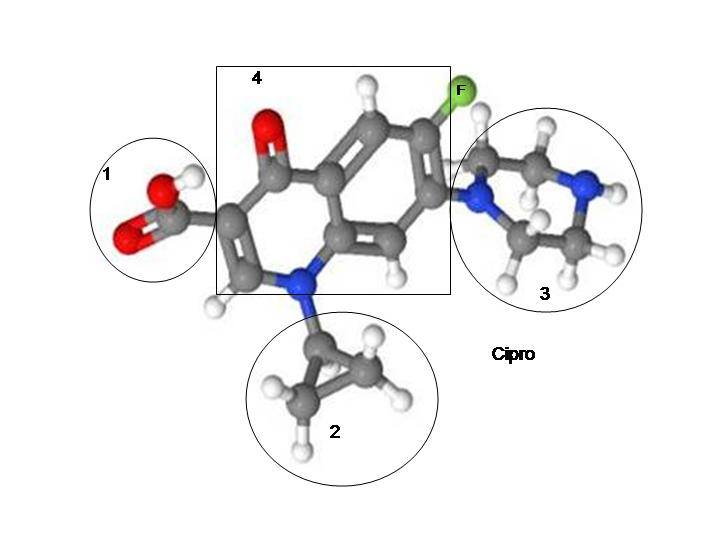
Kim looked at every gene linked to Charcot–Marie–Tooth – there are more than 40 overall, each one imparting a slightly different character to the disease. One leapt out: LMNA, which codes for a group of rope-like proteins that mesh into a tangled network at the centre of our cells. This ‘nuclear lamina’ provides cells with structural support, and interacts with a bunch of other proteins to influence everything from the packaging and activation of genes to the suicide of damaged cells. Given this central role, it makes sense that mutations in LMNA are responsible for at least 15 different diseases, more than any other human gene. These laminopathies comprise a bafflingly diverse group – nerve disorders (like Charcot–Marie–Tooth), wasting diseases of fat and muscle, and even premature ageing.
As Kim read about these conditions and their symptoms, she saw her entire medical history reflected back at her – the contracted muscles in her neck and back, her slightly misaligned hips and the abnormal curve in her spine. She saw her Charcot–Marie–Tooth disease.
She also saw a heart disorder linked to the LMNA gene that wasn’t ARVC but which doctors sometimes mistake for it. “Everything was encapsulated,” she says. “It was like an umbrella over all of my phenotypes. I thought: This has to be the unifying principle.”
Kim was convinced that she had found the cause of her two diseases, but the only way to know for sure was to get the DNA of her LMNA gene sequenced to see if she had a mutation. First, she had to convince scientists that she was right. She started with Grogan, presenting her with the findings of her research. Grogan was impressed, but pragmatic. Even if Kim was right, it would not change her fate. Her implant was keeping her heart problems under control, and her Charcot–Marie–Tooth disease was incurable. She didn’t see a point. But Kim did. “I wanted to know,” she says. “Even if you have a terrible prognosis, the act of knowing assuages anxiety. There’s a sense of empowerment.”
In November 2010 Kim presented her case to Ralitza Gavrilova, a medical geneticist at the Mayo Clinic. She got a frosty reception. Gavrilova told Kim that her odds of being right were slim. “I got this sense that she thought I’d made an unfounded shot in the dark,” says Kim. “That I didn’t understand the complexity of the genome. That I had been reading the internet, and they come up with all sorts of things there.”
Gavrilova pushed Kim towards a different test, which would look at seven genes linked to ARVC. Her insurance would cover that, but if she insisted on sequencing the DNA of her LMNA gene, she would have to foot a $3,000 bill herself. Why waste the money, when it was such an unlikely call? But Kim was insistent. She knew that the known ARVC genes explain only a minority of cases and that none of them was linked to neural problems. In all her searching she had found only one that covered both her heart and nervous problem. Eventually, Gavrilova relented.
Kim, meanwhile, disappeared down to Baja in Mexico. Gavrilova’s scepticism had worn her down and she fully expected that the results would come back negative.
When she returned home in May, there was a letter waiting for her. It was from Gavrilova. She had been trying to call for months. The test had come back positive: on one of her two copies of LMNA Goodsell had a mutation, in a part of the gene that almost never changes. LMNA consists of 57,517 DNA ‘letters’, and in the vast majority of people (and most chimps, monkeys, mice and fish) the 1,044th position is filled by a G (guanine). Kim had a T (thymine). “All evidence suggests that the mutation found in this patient might be disease-causing,” Gavrilova wrote in her report.
In other words, Kim was right.
“I’m beyond impressed,” says Michael Ackerman, a geneticist at the Mayo Clinic. He specialises in inherited heart disorders like ARVC that can cause sudden death at any time. Such diseases make for people who do their homework, but Ackerman describes most as “Google-and-go” patients who check their diagnosis online, or read up about treatment options. Kim had written up her research as a white paper – 36 pages of research and analysis. “Kim’s the only one who handed me her own thesis,” he says. “Of all the 1,000-plus patients I’ve taken care of, none have done extensive detective work and told physicians which genetic test to order.”
He thinks she nailed it too. It is unlikely to be the whole story – Kim almost certainly has other mutations that are affecting the course of her disease – but LMNA “is certainly the leading contender for a unifying explanation, without there being a close second,” he says. “The evidence is pretty good for this being a smoking gun.”
The test had vindicated her hypothesis, but it also raised some confusing questions. Heart problems are a common feature of laminopathies, but those mutations had never been linked to ARVC, Kim’s specific heart malfunction. Had she been misdiagnosed? A few months later, Kim stumbled across a new paper by a team of British researchers who had studied 108 people with ARVC and found that four had LMNA mutations (and none of the standard ones). “To the best of our knowledge, this is the first report of ARVC caused by mutations in LMNA,” they wrote. They didn’t know about Kim’s work – they couldn’t have, of course. But she knew. Kim had beaten them to it. “I was so excited, I was running up and down the beach,” she says.
When patients get solutions to their own genetic puzzle, it’s always professional geneticists who do the solving. Take James Lupski. He has been studying Charcot–Marie–Tooth for decades, and discovered the first gene linked to the condition. He also has it himself. In 2010 he sequenced his own genome and discovered a previously unidentified mutation responsible for the disease. In other cases anxious parents have been instrumental in uncovering the causes of their kids’ mysterious genetic disorders after long diagnostic odysseys, but only by bringing their cases in front of the right scientists.
Kim, however, was an amateur. And to her, sequencing was not a Hail Mary pass that would – maybe, somehow – offer her answers; it was a way of confirming a carefully researched hypothesis.
“People have been talking about empowering consumers since there was an internet,” says Eric Topol, a geneticist at the Scripps Clinic. “But finally, we’ve reached a point where someone can delve into their condition beyond what the top physicians at the Mayo Clinic could. They couldn’t connect the dots. She did.”
Topol, a self-described “digital medicine aficionado”, argues that Kim is a harbinger of things to come. In his book The Creative Destruction of Medicine, Topol foretells a future where doctors are no longer the gatekeepers of medical information. Advances like personal genetic testing or sensors that measure molecules in the blood will give patients the power to better understand themselves and to exercise more control over their healthcare. Medicine is becoming more democratic.
Kim is a vanguard of that change. She lacked academic knowledge, but she had several advantages over her physicians and other researchers in the field. She had detailed first-hand knowledge of her own symptoms, allowing her to spot connections in the scientific literature that others had missed. She could devote hours to learning everything about her niche disorders – time and focus that no clinician could reasonably spend on a single case. And she had unparalleled motivation: “There’s nothing that engages your curiosity more than being confronted by your death,” she says.
It is also becoming ever easier for that curiosity to lead to discovery. In the past geneticists would try to diagnose patients by looking at their medical history and deciding which genes might be worth sequencing, as Gavrilova tried to do for Kim. The approach makes sense, but it only ever confirms known links between genes and diseases.
One way of finding new links is to sequence a patient’s exome – the 1 per cent of their genome that contains protein-coding genes. It’s cheaper than sequencing a full genome, but allows researchers to hunt for disease-related genes by interrogating every possible suspect simultaneously, without having to whittle down the list first. “Suddenly, we’re finding patients presenting with Disease X who have mutations in genes never previously associated with that disease,” says Daniel MacArthur, a geneticist at Massachusetts General Hospital. “That’s happening in nearly every disease field right now.”
Exome sequencing is now barely more expensive than sequencing much narrower gene panels. MacArthur says that the cost has already fallen below $1,000 and may halve again this year. And once patients have that information, they could use it to find others with the same mutations and check if they have the same symptoms.
Currently, the results from DNA sequencing studies are largely squirrelled away in boutique databases that collate mutations for specific diseases or genes. The ironically named Universal Mutation Database covers mutations in only 34 genes, including LMNA. Broader ones exist, but for decades they have been incomplete, rife with mistakes, or inaccessible, even to other researchers – a sad state of affairs that MacArthur laments as the “single greatest failure in human genetics”. Now, though, the National Institutes of Health are developing an open database called ClinVar that covers all disease mutations. “A lot of us are putting our hopes on this,” says MacArthur. “We need to come up with resources that empower people to make surprising links, which is hard to do if the data are broken up by disease or gene.”
But for every Kim, there are others who research their own conditions and come up with wrong answers. In one study four non-specialist volunteers tried to diagnose 26 cases from the New England Journal of Medicine by Googling the symptoms. They got less than a quarter right. Genetic diseases arguably lend themselves to confusion and misinformation. They are often both debilitating and enigmatic, and getting sequenced can offer little comfort beyond a diagnosis. If mainstream science has no easy answers to offer, many patients will follow any lead, no matter how weak. “There’s a tendency for people to spin very convoluted stories on tenuous threads of evidence. Even scientists do that,” says MacArthur. “I have heard of a lot of rare-disease patients who come up with hypotheses about their disease, and very few turn out to be correct.”
Even Kim’s tale could have taken a different turn. Last year, a team from the Baylor College of Medicine sequenced the exomes of 250 people with suspected genetic disorders, and found that four of them had two diseases caused by mutations in different genes. In other words, Kim’s hunch about her two diseases sharing a common root could well have been wrong. Lightning does occasionally strike twice.
“We almost always have to spend time with patients decoding and recoding the impression that they’ve acquired about their disease from their own homework,” says Ackerman. Kim was an exception, he says, and her other physicians echo that view. She is unique. She is one-of-a-kind. She is extraordinary. High praise, but it conceals the implicit suggestion that she is an outlier and will continue to be.
“Bullshit,” says Kim. “I hear this all the time: that I’m an exception. That the patient of the future is not going to do what I did.” She bristles at the very suggestion. “I almost take offence when I hear that what I’ve done is exceptional.”
We are talking over coffee at La Ventana. This is her fifth winter here, and she and CB have just celebrated their 30th wedding anniversary. CB leans back against a wall, quiet and contemplative. Kim sits forward, animated and effusive. She’s drinking decaf because of her heart, but it’s not like she needs the caffeine. “Take Rodney Mullen. He’s a real genius,” she says. Mullen is not a figure from science or medicine. He is, in fact, a legendary skateboarder, famous for inventing mind-blowing tricks that previously seemed impossible. One of them is actually called the ‘impossible’. “He executes these movements that defy reason, films them and publishes them on YouTube,” Kim says. “And inevitably, within a few weeks, someone will send him a clip saying: This kid can do it better than you. He gave that trick everything he had, he’s pulling from all of his experience, and here’s this kid who picks it up in a matter of weeks. Because he learned that it’s possible to do that. Rodney just acts as a conduit. He breaks barriers of disbelief.”
Her protestations aside, Kim is unique. Throughout her life she had built up a constellation of values and impulses – endurance, single-mindedness, self-reliance and opposition to authority – that all clicked in when she was confronted with her twin diagnoses. She was predisposed to win. Not everyone is. But as genetic information becomes cheaper, more accessible and more organised, that barrier may lower. People may not have to be like Kim to do what she did.
Kim isn’t cured. Her LMNA discovery offered her peace of mind but it did not suggest any obvious treatments. Still, she has made a suite of dietary changes, again based on her own research, which she feels have helped to bring her nervous symptoms under control. Some are generic, without much hard science behind them: she eats mostly organic fruit, vegetables, nuts and seeds, and avoids processed food. Others are more tailored. She drinks ginger tea because it thins the blood – she says that many people with laminopathies have problems with clots. Whether her choices are directly slowing the progress of her diseases or triggering a placebo effect, she is fit and happy. Her defibrillator hasn’t shocked her in months. And, of course, she still exercises constantly.
Up the hill from the beach we can see the little yellow house where she wrote the 36-page booklet that put together all her research. It convinced her doctors, yes, but it did even more. She showed it to her brother, now an anaesthesiologist, and it allowed them to reconcile. “It’s like I’ve finally done something worthy with my life,” Kim says. “He told me I’d done some really good research and that I’d missed my calling as a medical researcher. I told him I think I’ve been doing exactly what I needed to do.”
This article first appeared on Mosaic and is republished here under a Creative Commons licence.










… [Trackback]
[…] Read More on that Topic: floxiehope.com/fluoroquinolones-and-epigenetic-triggers-possible-connections-with-charcot-marie-tooth-disease/ […]
… [Trackback]
[…] Information to that Topic: floxiehope.com/fluoroquinolones-and-epigenetic-triggers-possible-connections-with-charcot-marie-tooth-disease/ […]
… [Trackback]
[…] Information on that Topic: floxiehope.com/fluoroquinolones-and-epigenetic-triggers-possible-connections-with-charcot-marie-tooth-disease/ […]
… [Trackback]
[…] Find More on on that Topic: floxiehope.com/fluoroquinolones-and-epigenetic-triggers-possible-connections-with-charcot-marie-tooth-disease/ […]
… [Trackback]
[…] There you will find 17072 additional Info to that Topic: floxiehope.com/fluoroquinolones-and-epigenetic-triggers-possible-connections-with-charcot-marie-tooth-disease/ […]
… [Trackback]
[…] Find More on to that Topic: floxiehope.com/fluoroquinolones-and-epigenetic-triggers-possible-connections-with-charcot-marie-tooth-disease/ […]
… [Trackback]
[…] Information to that Topic: floxiehope.com/fluoroquinolones-and-epigenetic-triggers-possible-connections-with-charcot-marie-tooth-disease/ […]
… [Trackback]
[…] Information on that Topic: floxiehope.com/fluoroquinolones-and-epigenetic-triggers-possible-connections-with-charcot-marie-tooth-disease/ […]
… [Trackback]
[…] Read More Info here on that Topic: floxiehope.com/fluoroquinolones-and-epigenetic-triggers-possible-connections-with-charcot-marie-tooth-disease/ […]
… [Trackback]
[…] Read More Information here on that Topic: floxiehope.com/fluoroquinolones-and-epigenetic-triggers-possible-connections-with-charcot-marie-tooth-disease/ […]
… [Trackback]
[…] Find More Info here on that Topic: floxiehope.com/fluoroquinolones-and-epigenetic-triggers-possible-connections-with-charcot-marie-tooth-disease/ […]
… [Trackback]
[…] Read More on that Topic: floxiehope.com/fluoroquinolones-and-epigenetic-triggers-possible-connections-with-charcot-marie-tooth-disease/ […]
… [Trackback]
[…] Find More here to that Topic: floxiehope.com/fluoroquinolones-and-epigenetic-triggers-possible-connections-with-charcot-marie-tooth-disease/ […]
… [Trackback]
[…] Find More here on that Topic: floxiehope.com/fluoroquinolones-and-epigenetic-triggers-possible-connections-with-charcot-marie-tooth-disease/ […]
… [Trackback]
[…] Information on that Topic: floxiehope.com/fluoroquinolones-and-epigenetic-triggers-possible-connections-with-charcot-marie-tooth-disease/ […]
… [Trackback]
[…] Read More here to that Topic: floxiehope.com/fluoroquinolones-and-epigenetic-triggers-possible-connections-with-charcot-marie-tooth-disease/ […]
… [Trackback]
[…] Information on that Topic: floxiehope.com/fluoroquinolones-and-epigenetic-triggers-possible-connections-with-charcot-marie-tooth-disease/ […]
… [Trackback]
[…] Read More on on that Topic: floxiehope.com/fluoroquinolones-and-epigenetic-triggers-possible-connections-with-charcot-marie-tooth-disease/ […]
… [Trackback]
[…] Read More on to that Topic: floxiehope.com/fluoroquinolones-and-epigenetic-triggers-possible-connections-with-charcot-marie-tooth-disease/ […]