Scott suffered his health battles and decided to take his health into his hands and do the research and get a team of knowledgeable people to assist him. I see many similarities in my story, and that is why I think so highly of Scott and his movement.
Recently, Scott and I talked about doing a podcast around fluoroquinolone toxicity and fluoroquinolone treatment and how Floxie Hope has been a beacon of hope. Scott was kind enough to spread that message on his show with another guest, Dr. Mark Ghalili who treats these issues as well.
Please have a look at the show on Scott’s webpage.
Please keep the comment section free of negative statements, Floxie Hope is intended to help keep hope, not hate.
Fluoroquinolone toxicity & treatment takeaways from the show
Alot of what we spoke about in the show was around what toxicity looks like and how it happens.
We discussed my personal symptoms and story and how some simple interventions could have changed my health in a big way.
This podcast also touches Dr Ghalili’s experience with the drug and how he assists patients in regaining their health.
I hope that this podcast serves to help though who suffer from fluoroquinolone toxicity from Cipro, Levaquin or Avelox. I am doing everything I can through Floxie Hope to spread the word, but I need your help to get the message out to those who need it. Please keep hope and know you will get better.
Transcript from Scott’s Podcast
Transcript Disclaimer: Transcripts are intended to provide optimized access to information contained in the podcast. They are not a full replacement for the discussion. Timestamps are provided to facilitate finding portions of the conversation. Errors and omissions may be present as the transcript is not created by someone familiar with the topics being discussed. Please Contact Me with any corrections. (Disclaimer from Scott at better health guy)
[00:00:01.13] Welcome to BetterHealthGuy Blogcasts, empowering your better health. And now, here’s Scott, your Better Health Guy.
[00:00:15.10] The content of this show is for informational purposes only and is not intended to diagnose, treat, or cure any illness or medical condition. Nothing in today’s discussion is meant to serve as medical advice or as information to facilitate self-treatment. As always, please discuss any potential health-related decisions with your own personal medical authority.
[00:00:35.11] Scott: Hello everyone, and welcome to episode number 146 of the BetterHealthGuy Blog casts series. Today’s guests are Dr. Mark Ghalili and Jason Sousa, and the topic of the show is Fluoroquinolone Toxicity.
Dr. Mark Ghalili is a regenerative medicine specialist at Regenerative Medicine LA. He pursued his undergraduate studies at the University of California Irvine and then went on to obtain his medical degree at Western University of Health Sciences. As a regenerative medicine specialist, Dr. Ghalili’s passion lies in teaching his patients about chronic disease, prevention, and finding the underlying reasons for their illness.
Unfortunately, a monumental event in his own personal life changed his path forever. In late 2016, Dr. Ghalili experienced a severe and common adverse reaction to a widely prescribed antibiotic called Cipro. On his second day of antibiotic treatment, he found himself grasping for life in excruciating pain, and this was only the beginning of an onslaught of symptoms that changed his life forever.
Dr. Ghalili soon suffered from complete muscle wasting, burning neuropathy, seizures, brain fog, vertigo, blurry vision, and tendon tears in his legs. His life became confined to a wheelchair, crippled, and unable to walk. Dr. Ghalili’s only hope was implementing alternative and regenerative therapies, as the traditional medical doctors had no answers for him, nor did they even believe him.
Dr. Ghalili went from being confined in a wheelchair, unable to treat patients, living in excruciating pain, to gaining the gift of running again, something he will never take for granted. Dr. Ghalili was persistent to gain his normal life back, so he could help millions around the world.
Jason Sousa is a patient advocate and editor of FloxieHope.com. His own health took a sharp decline six months after using a fluoroquinolone antibiotic in 2013.
Today, Jason works tirelessly to help others that have been floxed to improve their quality of life and to put an end to their suffering by sharing knowledge and stories of hope. And now, my interview with Dr. Mark Ghalili and Jason Sousa.
The topic of fluoroquinolone toxicity, or what’s known as floxing, is one that I’ve wanted to talk about on the podcast for some time.
Many of our listeners have dealt with chronic Lyme disease, and fluoroquinolone antibiotics are commonly used in that realm, particularly with the co-infection Bartonella. I personally was on Levaquin for about three months over a decade ago, and even though I didn’t have any obvious floxing symptoms, you have to wonder what damage these drugs may have caused even when it may not be entirely clear. Thanks so much for being here today to talk about this important topic Dr. Ghalili and Jason.
[00:03:33.23] Dr. Ghalili: Thank you for having us Scott, it’s a pleasure.
[00:03:35.27] Scott: Thank you.
[00:03:36.18] Dr. Ghalili: Love your work.
[00:03:37.11] Scott: Thanks so much. Let’s start by talking about how you became interested in the topic of floxing; what was your personal experience that led you to making this area such a personal passion today?
[00:03:48.26] Dr. Ghalili: So I was a floxed myself, working as a traditional medical doctor at one of our prestigious hospitals here in Los Angeles, and it gave me an awakening and made me realize how corrupt the pharmaceutical industry is. And how people have been damaged for over 30 years by this class of antibiotics.
So if it didn’t happen to me, I probably wouldn’t be as passionate about it. But when you actually live through something, and you see other people suffering through a similar circumstance, it becomes personal to you. So the way I practice medicine it’s very personal; it’s not just another patient. Because I look at everyone as if they’re myself because they’re dealing with the same thing I dealt with.
[00:04:26.16] Jason S.: Yes, for me, it became my life’s work because it hit me so hard in my late 20s. And I had no idea what was going on, and doctors weren’t giving me the answer, so I had to be my own doctor. You find a lot about yourself going through a health challenge, and I see so many thousands of people that go through this and don’t know how to explain it.
So doing everything I can to spread awareness and spread knowledge and hope to people so that they know that they can get help and they can get better. There is people working on this that can help, so.
[00:05:00.26] Scott: Being a part of a community like chronic Lyme disease or Chronic Fatigue Syndrome, CFS/ME or mold illness or Morgellons or PANS/PANDAS, people are often told that these conditions are psychological. What do you say to those that suggest that floxing is not a physiological condition but rather a psychological one?
[00:05:22.18] Dr. Ghalili: Well, that’s a great question, Scott. It’s actually a little bit of both. But what I can tell you is people don’t fly from all over the world and pay out of pocket for treatment that their insurance does not cover if they don’t actually feel something is wrong with them. That’s the first thing I’ll tell any doctor.
Nobody’s going to come sell their house and not be able to work for months just to come and get treatment; it doesn’t make any sense. So there is a psychological aspect as well because these drugs damage your central nervous system, which we’re going to discuss more in-depth moving forward with this discussion.
[00:05:57.00] Jason S.: For me, I feel that there’s a cause, and then you have an effect, right? These people have a normal healthy life. They get a prescription, they fill the prescription, they take that prescription, and they start to fall apart. They notice their body’s falling apart, they notice they’re having tendon problems and all of these other problems they’ve never had in their life, and then all of a sudden, it becomes psychological.
The fear, the panic. They go to the doctor; the doctor can’t explain it. So it’s specialist after specialist with no answers. So it actually compounds that psychological process and the fear mentality, and yes, it’s overwhelming for sure. And that acute phase after you take that prescription.
[00:06:36.29] Dr. Ghalili: I would also like to add there is gaslighting by the medical industry because they’re the ones prescribing the medication. They don’t want any trouble; they don’t want to get sued. So they’re always going to deny the fact that these drugs can have that effect.
[00:06:49.16] Scott: So speaking of these drugs, what are some of the medications that people should be aware of that are commonly used in this class that can lead to potential problems, including floxing?
[00:07:00.10] Dr. Ghalili: Yes. So, Cipro, as we know, is the most popular drug or ciprofloxacin; its cousin Levaquin is even more toxic. And my experience Avelox or moxifloxacin is probably the most toxic of them all. But you also need to realize they have eye drops, Ciprodex which is Cipro combined with dexamethasone steroid. That they give to kids ear drops, eye drops and those can be very harmful as well.
[00:07:25.01] Scott: So what are these medications commonly used for, are there in some cases no other alternatives to using them? Are they potentially the only solution for an infection? And are there conditions where you would consider using these medications?
[00:07:40.21] Dr. Ghalili: Personally, from my medical experience, over 850 patients that we’ve seen, treated, or spoken to with fluoroquinolone toxicity, I have yet to see one patient to show me one culture showing sensitivity to these drugs. Every single one of my patients I’ve ever seen or spoken with was prescribed this class of antibiotics for no legitimate reason, without due diligence.
There were other options for every single one of those patients, and maybe one or two patients actually had a confirmed bacterial infection that I’ve seen in my whole career that were prescribed as passive antibiotics. And for those two patients, their culture had another option of what they could have used instead.
[00:08:23.12] Scott: So how commonly might these medications then lead to complications in your experience? And are these complications more common in men or women? When did we in history seem to start seeing the fluoroquinolone toxicity problem emerging?
[00:08:39.26] Dr. Ghalili: I believe it started in the late 80s, early 90s when Cipro became eminent, and they’re using in the Gulf War for Gulf War Syndrome for patients that were possibly exposed to anthrax. And that’s why we have, in my opinion, the Gulf War Syndrome was exacerbated by taking this antibiotic for over 40 days.
I don’t have an exact percentage per se, to say this many percentages of people get injured because the injuries are different. When you’re talking mitochondrial damage, I feel every single patient who takes this pill; it’s a toxic pill, uses a chemotherapy agent, will have some sort of damage or genetic changes, because let’s say your body’s at a hundred percent and you go down to eighty percent, you’re still functioning properly.
You don’t notice you have these side effects. But once you get down to forty, thirty percent of your functional capacity, you’re going to start feeling the aches, the pains, and you’re going to have these debilitating symptoms. But it’s a gradual effect, so every time you take it, you’re damaging your mitochondria more and more and more.
So it’s difficult to tell you how many percent of people have side effects; which side effect? Neurological, musculoskeletal, neuropathy, there are so many different side effects that can occur. But it’s patients that have pre-existing conditions or that have other injuries in the past. Or you give a patient who’s taking chemotherapy, and you give them Cipro 10 years later, well it’s not going to turn out well, that one pill is not going to turn out well.
You can give somebody 20, 30 pills. They might still feel okay; they might be able to excrete, they have a good genetic profile. But even that person, the healthiest person on earth over time, is going to have their mitochondria deteriorate with this class of antibiotics. The reason is so it’s more common in women, and I’ll tell you why; the reason it’s more common in women is because Cipro’s prescribed and Levaquin in a 4:1 ratio women compared to men, 4 or 5 to 1 ratio. So for every like five women who take Cipro, one man is taking it.
Why? Because of UTIs. Women are more prone to UTIs. Women are more prone to this Chronic Fatigue Syndrome, Fibromyalgia. Women get gaslighted more in the medical industry, right? You’re crazy; it’s in your head, you’re anxious, you’re depressed, take an antidepressant. Men don’t really go to doctors as often and say, hey, I want to take care of my health.
Men are just like, oh whatever; I’ll deal with it. So that’s why in my opinion, women are floxed more than men. But, men can tend to fare better because of things like testosterone, like being able to have energy, muscle strength. Men have more muscle tone than women do.
So for women who take this, they’re more prone to have their muscles get damaged because they don’t have the same muscle tone and structure that men do.
[00:11:23.23] Scott: So what are then some of the symptoms that one should watch for if they’re using these medications? What are some of the issues that can arise from using fluoroquinolones and potentially becoming floxed? And is the damage specific to the tendons, or can it impact potentially the entire body?
[00:11:41.02] Dr. Ghalili: I want Jason to answer this first because he also dealt with it himself. And I’d love for him to give his personal insight of what he dealt with for so many years.
[00:11:49.01] Jason S.: So it basically starts off being healthy and then filling a prescription. For me, I had what is called a delayed reaction. I was 28, as an athlete, in the gym six days a week, very physically fit, and this is coming off a Lyme diagnosis, rounds of antibiotics. A few months later, suspected epididymitis; here are 30 days of Cipro.
Let’s knock it out; it did knock it out. I made it to pill 27 just kind of gave up on it. And then at the gym, like five months later, six months later, just popped my piriformis muscle. Went to the emergency room; I was really anxious, had a lot of anxiety. Gave me Lorazepam Ativan, which calmed me down, which is pretty much a no-no to do when you have fluoroquinolones. But I was calm, had a tons of pain, the next day lost my ability to walk, trouble breathing.
Some psychotic episodes, depression, depersonalization like just anxiety through the roof, and really just body-wide nerve pain. And that continued for a few months until I started to find any doctor that would help me. I found a Lyme literate doctor; he knew I had Lyme, just gave me some nutritional IVs, which got me a little bit better, but these symptoms continued for years and years on and off when I would do physical activity or get in high-stress situations.
My tendons would get tight and lose my ability to walk functionally; anxiety would come back, insomnia would come back years after taking the drug. And the delayed reaction was shocking to me because I had no idea that the antibiotic had caused that reaction so far out.
I figured watch out for the black box warnings, Achilles rupture, okay nothing happened, six months later I fell apart, I had no idea. I thought it was just Lyme disease, but according to a lot of thousands of people on Facebook, it was an antibiotic.
[00:13:46.19] Dr. Ghalili: And I would like to add additional symptoms like Jason mentioned, you have brain fog, memory loss, depression, anxiety, paranoia, hallucinations, panic attacks. I’ve seen patients be suicidal.
They go into psychosis, restlessness. They get palpitations, which are very common, especially in the first 30 days. Agitation, anxiety, confusion, brain fog, delirium, muscle wasting, tendon pain, tendinosis, joint popping is very common as well.
Blurry vision, and just this chronic fatigue. And that’s what we mainly see in the office when patients complain about fluoroquinolone toxicity.
[00:14:30.21] Scott: So you’ve hinted at the idea that when these symptoms appear can be varied, can be early, can be later. But let’s talk about that a little bit more, so how long does it generally take to see some symptoms of this fluoroquinolone toxicity?
Can it be right away? I’ve actually heard a story of a person who took one pill and was still having issues a year later. Can it take three to six months? Does it need to be a certain amount of these medications? Is it a cumulative effect? How much damage has to be done before the symptoms then present?
[00:15:04.12] Dr. Ghalili: So it can be immediate like you said, depending on the patient. Are they combining the fluoroquinolones with a steroid? It’s most likely going to be immediate. Are you combining with ibuprofen? More so than likely immediate. Is it your first time taking it? You’re young and healthy; you might not have an issue, right?
But over time, it can have a cumulative effect. You might take Cipro and one year later have a steroid injection in your shoulder, bomb will go off in your body, right? And we can attribute that to if you may have never taken that fluoroquinolone, and you have that storage shot, you may have been okay.
So I’ve seen every single type of patient, some patients will take like a cumulative effect, but they don’t necessarily have a bomb go off in their body. They’re just always chronically fatigued; they’re tired. Then you ask them, oh yes, I’ve had seven rounds of Cipro from 2002 to 2015. And ever since these last seven or eight years, I’ve just been feeling really tired and fatigued, and my muscles ache, I can’t work out.
You get those patients as well that don’t even know a bomb went off in their body; it’s just a slow, gradual mitochondrial decline.
[00:16:10.20] Scott: You have said that fluoroquinolones are the number one cause of Chronic Fatigue Syndrome; tell us a little more about that. Do we know the percentage of, or do you have some speculation around, the percentage of people with Chronic Fatigue Syndrome or ME that had prior use of fluoroquinolones?
[00:16:28.24] Dr. Ghalili: So there’s no specific data on that, but what I can tell you is if you ask patients with Chronic Fatigue Syndrome, and this is not to say all of them. Chronic Fatigue Syndrome is a blanket diagnosis doctors will give when they can’t figure something out. Oh, you have Chronic Fatigue Syndrome. In my expert medical opinion, I believe Chronic Fatigue Syndrome is caused by mitochondrial dysfunction.
If you can’t produce ATP properly, which is the precursor for energy in the system. Well, if you have no energy, you will be chronically fatigued. So what’s preventing your cells from producing the right amount of ATP? Mitochondrial stress and damage. I don’t have specific data on that because what do you define as Chronic Fatigue Syndrome?
What level of fatigue, everyone’s level of fatigue is different. So for me, tired is going to be different than somebody else who says I’m tired. So it’s pretty much impossible to get data on that. But if you do have patients with that diagnosis, and you ask them, have you ever taken Cipro, Levaquin, fluoroquinolone?
You’ll be surprised the overwhelming majority will be like, well, yes, I did. Yes, I’ve had steroids. I do take ibuprofen all the time, or you’ll find other fluoridated medications that can cause that type of mitochondrial damage as well. And once you figure that out, you’ll understand why they have this diagnosis.
[00:17:43.05] Scott: Are there conditions that might increase the risks associated with these medications? And then extending on that discussion, if we look at the genetic predispositions or the SNPs, for example. Are there certain genes that might be associated with a worse outcome when using these medications?
[00:18:00.22] Dr. Ghalili: Yes, so I think so. I think anyone with autoimmune disease should not be taking this class of antibiotics. It can lead to, we’ll get into this, but the leaky gut situation and the potential to worsen autoimmune conditions. Any type of skin disorders like Marfan syndrome, Ehlers-Danlos Syndrome. I’ve had multiple patients with EDS one pill of Cipro; they’re done.
Because they already have issues with their collagen. And these drugs will attack; when you have an issue somewhere already, that’s where it’ll attack. If you’ve had a knee surgery, and you go and take this antibiotic, you’re going to start feeling pain in that knee you have surgery on because there’s already been damage there; it’s already compromised.
So I wouldn’t take it if you have any of those type of conditions. You brought up genes which are very important. Many of my patients have an MTHFR, which is methyl tetrahydrofolate reductase reduced activity. And they can’t methylate properly. So that impairs their detoxification pathways, they can’t detox properly. It might take them a little more time to get rid of the toxins and the aldehydes caused by the fluoroquinolones.
So those patients get an excessive buildup and can be floxed faster, in my opinion, than others. You also have glutathione as transferase, glutathione we know is a master antioxidant of the body. So if you have reduced levels of glutathione in your body, you’re impairing your detoxification pathways. You can’t get rid of the toxic chemicals; as part of the reaction that the fluoroquinolones create, SOD2 is superoxide dismutase.
That is an amazing antioxidant that your body produces and prevents aging from happening. So if you have a deficiency in that, it can weaken your cells. Vitamin D receptors, those patients just have, their receptors not uptaking vitamin D properly, so tend to have lower vitamin D levels. And we know how important vitamin D is to our health and well-being.
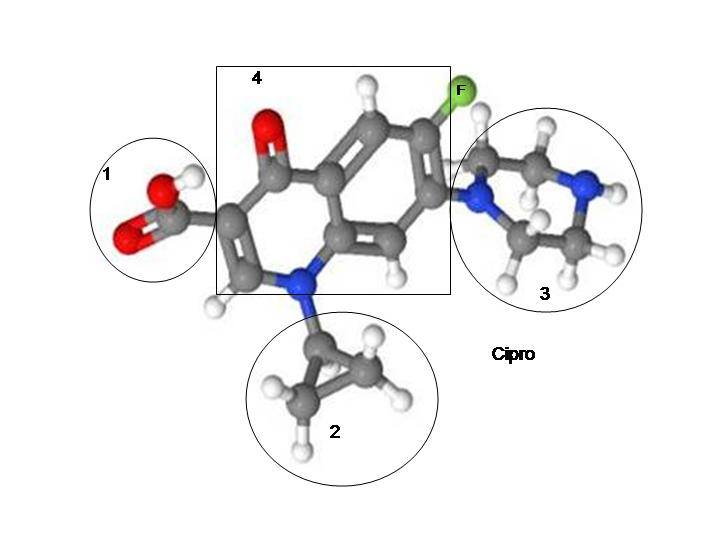
[00:19:56.23] Scott: What is the intended mechanism of action of these medications? And do they impact human cells in a similar way as they are supposed to impact the bacterial cells?
[00:20:08.27] Dr. Ghalili: So I think every Floxie, including Jason, will agree with this. But these antibiotics not only damage your bacterial cells, which look, they do a great job at killing bacteria. I mean, you have an infection, you give someone this antibiotic. I’m not saying it doesn’t work; it works great. It’s just you’re using a machine gun to kill a fly when all you need is a flyswatter.
And that’s what I’m trying to say. They inhibit DNA gyrase or topoisomerase too, which can penetrate normal healthy cells. This is required for ATP production, so ATP produces energy. We also know that they chelate iron and magnesium, so they kind of remove iron and magnesium from your cells.
And these studies can show can lead to epigenetic changes and, obviously mitochondrial damage. And the way they do that is they cause peroxynitrite, which are toxic, and then they make aldehydes, and you get free radical damage, and ultimately the cell can just die. So you don’t have healthy mitochondria.
[00:21:13.03] Scott: Is there a lab test that we can do to show that someone was injured by these medications? Can we do a punch biopsy, for example, and see some difference in people who have been floxed?
[00:21:25.05] Dr. Ghalili: So I think Jason had a skin biopsy performed as well, and usually, the majority of patients that have a skin biopsy will show small peripheral fiber neuropathy, usually down in the legs. But things you can look at if you’ve taken the antibiotics, you look at your legs, and they look like a diabetic leg. Like a poorly-controlled diabetics leg.
Patients will not grow hair as fast in the lower extremity; you might see poor capillary refill, meaning it takes longer for blood flow to get back to the area. They have this smooth, dry, shiny skin appearance, and that’s due to the peripheral neuropathy that can be caused by these antibiotics.
So sometimes, you don’t really need to go down the route of having to take that skin biopsy; you can kind of get a glimpse from doing a physical exam as well. And if Jason wants to touch on that.
[00:22:13.02] Jason S.: Yes, I mean, it’s pathology, right? It’s just like the patient comes in with symptoms, and they had taken a drug, and any doctor could do a Google search and really look at clinical peer-reviewed evidence of the effects of these drugs.
And you don’t need anything invasive like a muscle punch biopsy to determine small fiber neuropathy. It’s an invasive way to do it, but most floxies do have small fiber neuropathy at some point. So it’s just listening to the patient and just working on rebuilding the system that’s been so damaged by this class of drugs.
[00:22:45.09] Scott: In patients that have had an adverse reaction to fluoroquinolones, are there some labs that you might use to more broadly explore how to potentially help them in a more holistic manner?
[00:22:57.05] Dr. Ghalili: Yes. I’ve treated many patients without labs because you’re not going to find specific lab tests that will prove fluoroquinolone toxicity. There are certain things that I see and I notice in patients who are floxed, but everyone’s floxed differently. You have even a majority of patients with completely normal labs.
What I have seen specifically in males also females are hormone levels change. So low testosterone is a big key, low T, high sex hormone-binding globulin. Low free testosterone, I see the magnesium levels. And doctors test the wrong type of magnesium, so we’ll test a regular magnesium level say, oh, your magnesium’s normal, you don’t need any, you’re perfect.
But red blood cell magnesium is a right test to do, and a lot of doctors don’t do that. Usually, initially, I’ll see false ANA readings, where the labs will tell you have an autoimmune disease. But usually, after a few months, that will dissipate and come back as normal. You want to check your thyroid levels; serum iron as well, due to chelating iron.
Like sometimes, looking at homocysteine levels, none of these really change my management per se. They can just kind of give me an idea of what’s going on, but it’s not going to change management. Homocysteine levels are a marker of inflammation. If those are high, patients most likely will have an MTHFR mutation because they can’t methylate and have high homocysteine levels.
Histamine levels, histamine levels can be up because you got that leaky gut. You eat certain foods, sparks a reaction, histamine goes up, so I tend to see that as well.
[00:24:31.28] Scott: One of the things that I learned as I was preparing for this conversation was that the “fluo” in fluoroquinolone is fluoride. So how much of the complication from these medications are associated with fluoride?
[00:24:44.00] Dr. Ghalili: Great question. If there’s no fluoride in the medication, I don’t think it causes the same damage. The fluoride is the most polarized molecule nature, has a strongest negative charge. So it can bind deep within the mitochondria into your cells; that’s how it penetrates the central nervous system.
That’s how antidepressants work; they have fluoride in them to penetrate the central nervous system. Some steroids have it in them, drugs like Lipitor or Crestor, statins have them in them, there’s a whole list of drugs of fluoride in them.
And drugs like fluoride, in my opinion, have the worst side effects; they cause the most damage. And the fluoride is what leads the drug to get into your cell, and that’s how it penetrates.
[00:25:24.00] Scott: Do we need to be concerned about other non-fluoroquinolone medications that might also contain fluoride like Prozac, for example. And then are there other medications or factors that increase the potential for a bad outcome? You’ve already mentioned steroids. But are there certain scenarios where we’re setting the stage for bigger problems?
[00:25:44.18] Dr. Ghalili: Yes, there are tons of drugs. Where if you take in the fluroquinolone antibiotics, and you take like an NSAID after, Ibuprofen, Motrin, Aleve, you can get re-floxed. You can have significant damage to your body; steroids are notorious. Steroids are more, they cause a lot of neurological side effects, neuropathy, and the tendon popping with tendinosis and potentially a tendon rupture.
There are SSRIs, as I just mentioned earlier; all have fluoride in them. I would avoid pretty much any drugs that have fluoride in them, the antidepressants, Prevacid, Protonix, statins, for example. It’s crazy I had a patient who was floxed; he was an HIV patient.
And I looked up every single HIV medication have significant high amounts of fluoride in them, and I just learned this recently too. Because you would never think, why would you give an HIV patient with a poor immune system fluoride every single day, and then wonder why they keep getting sick, right?
So you got to look at everything. Foods, things that have fluoride in them, you want to avoid toothpaste because there’s just no reason to keep putting that in your body once you’ve been floxed.
[00:26:58.29] Scott: So is the degree of damage then from the fluoroquinolones multifactorial? In other words, if someone’s using ibuprofen, or they’re using steroids, or they’re using antidepressants, or they’re using a combination of these things.
Does it then become exponentially more likely that they have problems with these medications?
[00:27:17.26] Dr. Ghalili: Yes. So the more fluoride exposure, like if you’re on an antidepressant for ten years and then take one or two pills of Cipro, that can do it. But if you did not take those antidepressants for ten years, you most likely would not have had that significant reaction from taking two pills. So it’s a cumulative effect, in my opinion from what I’ve seen, and I’ve treated hundreds of patients with this condition.
And I’ve noticed that combined with steroids is kind of really bad; combined with ibuprofen really leads to a lot of muscle and tendon issues. If you’re taking ibuprofen, steroids, antidepressants, you’re on PPIs; you’re on statins as well. Those patients are going to have stronger reactions on average than someone who’s not taking any meds at all, who just takes this for three days or five days for UTI.
[00:28:04.16] Scott: Another medication that I have commonly seen used in the chronic illness community is Diflucan, which also, to my surprise, I didn’t know it also contains fluoride. So can we have maybe a less severe presentation of floxing with something like Diflucan?
[00:28:21.19] Dr. Ghalili: Yes, Diflucan, I believe it’s triple fluoridated. There are three fluoride molecules in there, pretty strong. You can get re-floxed taking a Diflucan five years after you’ve been floxed, just from one pill. And also, Diflucan by itself, in my opinion, can cause issues like chronic fatigue, neuropathy, and neurological issues from what I’ve seen in the office.
[00:28:41.23] Scott: Let’s dig in a little bit more into the mechanisms, and you hit on some of these earlier. But what are the mechanisms that lead to damage in the body? How do these medications lead to long-term health complications? What’s actually happening?
[00:28:54.16] Dr. Ghalili: Yes. So long term, as we talked about, we believe it’s mitochondrial damage; that’s what all the studies are showing. When you’re chelating the magnesium out of the cells, you lead to deficiency.
And we know our cells all need magnesium in order to prosper and be healthy. The fluoride penetrates the central nervous system; as we said, it was the most polarized molecule in nature to do that. And long-term reason patients don’t get better is, we believe, due to epigenetic changes, DNA adduct formation where your DNA is being manipulated.
Because that’s what the drugs do to bacterial cells, and we hypothesize they’re doing that to healthy cells as well. So you’re having bad cells creating new bad cells; your body has turnover, right? Like your red blood cells turn over every 90 days, right? Your skin turns over. In a few years, pretty much every cell in your body turns over to a new cell. But why are Floxies damaged 10-20 years?
And so the only logical hypothesis you can explain is, you’re replicating a non-healthy cell to another non-healthy cell; that’s the only logical explanation I can make when your body makes a full turnover in about every seven years. Neurologically as well.
[00:30:07.22] Jason S.: The peroxynitrite formation too, that’s like a big deal, because there’s really no mechanism of action in the body that can protect itself from that. So without the use of like supplementation, it’s hard to stop that process, and it’ll just continually damage with like reactive nitrogen species. So like a lot of Floxies, don’t realize that, but it happens.
[00:30:27.18] Scott: So we’re talking then about dragging iron and magnesium out of the cell, which can inhibit the mitochondria, the peroxynitrite that you’re talking about here, that creates free radical stress. The production of aldehydes potentially as well.
So many different things that are happening here, besides what we normally think of with these medications, which is something happens to the tendons.
So let’s talk about that just a little bit; when we’re talking about tendons, is this a tendinopathy, or is this a tendinosis?
You have Dr. Mark called these medications “a blow torch to the tendons”, so why do most people experience the damage or think of the damage of these medications as tendon related when the impacts are really much broader?
[00:31:09.04] Dr. Ghalili: Yes, so the tendons usually go first, like so that’s the most common side effect, is your tendon, your Achilles tendon, why? So the Achilles has the poorest blood flow in the whole body. So if you’re not really getting oxygen there and all your nutrients and minerals to that area, it’s more prone to damage.
So once a drug can get in there, it chelates the magnesium out, but then you don’t have enough blood flow to replenish that magnesium and other minerals you need to the tendon, for example, right? And then we’re going to talk about proline and how that proline hydroxylase enzyme and how that gets blocked. It’s actually not a tendonitis; there’s zero inflammation going on.
And inflammation is, your body is sending signals cytokines to release inflammatory factors an inflammatory cascade that is not going on at all. You’re just taking minerals and nutrients out of these cells damaging the DNA. So it’s like taking a prune, and you’re drying it, so you’re drying that prune. You’re not really doing anything else to it versus attacking it and beating it up.
You’re not beating the prune up; you’re just drying it out; that’s exactly what’s happening to your cells. So it’s a tendonosis, not a tendonitis. If it was a tendonitis, and you gave steroids or ibuprofen, which are anti-inflammatory, you have resolution of symptoms, correct?
But you don’t; things get ten times worse. That’s my theory on why there’s no inflammation going on. You can measure CRP levels, ESR levels, which are markers of inflammation. 99% of the time, those are normal in floxed individuals.
[00:32:44.08] Scott: Is somebody who might already have lower iron or magnesium maybe because they’ve used it all up from dealing with chronic infections, for example. Are they at greater risk of problems when we’re talking about dragging out iron and magnesium? Or does this happen in people with normal iron levels at the same rate?
[00:33:03.04] Dr. Ghalili: I would say if you have mineral deficiencies, you’re more likely to have issues. Like for example, if we know their iron and magnesium chelators, well if you’re already low and we take out what you have, you’re more likely going to say, oh, you know my tendons are a little sore, oh I’m a little fatigued, oh my muscles are getting tight, right? So you want to replenish.
[00:33:23.00] Scott: How do these fluoroquinolones impact our collagen, our structural integrity. In the world of Lyme disease, collagen is already affected by Borrelia, for example. So how do the fluoroquinolones affect the collagen and structural integrity? And then you can maybe tie in that proline hydroxylase conversation in terms of the development and maintenance of collagen and tendons.
[00:33:44.20] Dr. Ghalili: Yes, great question. So we know fluoroquinolones can inhibit an enzyme called proline hydroxylase, and I’ve lectured about this before. That’s a precursor to collagen. We have several different types of collagen, focus on type one the skin, bones connective tissue, and cartilage. Type 2 is for the bone and joints, and type 3 is the muscles, organs, and blood vessels.
So when you’re damaging all of this, and you’re not able to create collagenous structures, well, that’s how you get the issues with the skin the drying of the skin, right? Patients can say, oh, I look aged, I look older. My connective tissue and cartilage, right? Knee joint popping, shoulder popping.
It also affects type 3, the muscles, which all your muscles and tendons get damaged. Your organs and blood vessels. Blood vessels is important because we know these drugs can increase the risk of aortic dissection, so they can cause a rupture in your aorta, which is seen on the black box warning as well.
[00:34:39.07] Scott: There seems to be a growing number of people dealing with hypermobility syndromes with Ehlers-Danlos Syndrome, which you mentioned earlier. What is the connection between fluoroquinolones and Ehlers-Danlos, for example?
Is it just that people with those conditions are more likely to be impacted when they then take fluoroquinolones? Or do you think the opposite also happens where maybe these medications are somehow triggering these conditions?
[00:35:04.25] Dr. Ghalili: So this brings up the same point as the magnesium, so you said if you have low magnesium, right? Are you going to have issues? Well Ehlers-Danlos same thing. So you’re already having issues with skin and collagen structure, mobility, right?
If you give the fluoroquinolone to a patient that already has damage done due to genetic reason, well, they’re just going to get wiped out because they already have an issue with that.
[00:35:29.05] Scott: In someone that’s dealing with, let’s say, chronic Lyme disease or mold illness, how do you differentiate the symptoms of fluoroquinolone toxicity versus the long list of things that can also present in those conditions?
[00:35:41.29] Dr. Ghalili: I want to defer this to Jason, he’s well versed in this, and he’s had to deal with these issues. So he’ll be able to give his insight and opinion based on his own personal experience. It should be great.
[00:35:55.05] Jason S.: So Scott, I’ve noticed running Floxie hope in a Facebook group. A lot of people in the fluoroquinolone community, Floxie community, have really bad gut issues, and it makes them more susceptible to getting mold in their body quite easily. And that is something I’ve had to deal with Stachybotrys and Aspergillus.
I used to live outside of Boston, had a basement, had water damage. And it got in, the mold, and it’s very hard to get out. I noticed that I had lingering symptoms, and they weren’t going away. So I knew I had to do some digging.
I noticed after reading Dr. Neil Nathan’s book that it became apparent that I needed to run an organic acid test, RealTime tests. See what mold I had in me, and I had skyrocket levels of Aspergillus and Stachybotrys. And it exacerbated all of my nerve symptoms, all of my fatigue. And I’ve noticed that it has happened to more fluoroquinolone patients and downstream to just having mold inside of my body. I was having oxalate issues.
So reactions to foods with high oxalates, pain in the joints, and from there, I started to get histamine intolerance. So I had almost like mast cell symptoms, and that didn’t really alleviate until I started to implement some of the strategies that Dr. Neil Nathan had proposed in his book, like get binders and do antifungals and get rid of the Candida and Aspergillus.
And the histamines started to get better, my tolerance for oxalate foods got better. But it’s pretty prevalent in the fluoroquinolone community, this whole mast cell-like symptom and mold issue for sure.
[00:37:36.17] Scott: So I think we know that mold exposure can be probably one of the more common triggers for mast cell activation, and many people listening to this have dealt with that to some degree. Is there a potential connection as well between the fluoroquinolones and the development of Mast Cell Activation Syndrome or histamine intolerance?
[00:37:57.04] Dr. Ghalili: I believe there is.
[00:37:58.04] Jason S.: In my opinion, I believe so.
[00:37:59.01] Dr. Ghalili: Yes. Because you can have patients with like high histamine levels, or they’re just allergic to everything. And we think that’s due potentially to a permeability leaky gut, which I know we’re going to talk about.
And there’s a reduced aldehyde dehydrogenase, so that can also lead to histamine intolerance for patients. And some patients may have a DAO gene, diamine oxidase enzyme deficiency, and then they have high histamine levels because of that, they can’t tolerate certain things. And they get triggered by certain foods as well.
[00:38:32.14] Scott: So let’s talk now about some of the supportive options, things people can explore. I want to make it really clear that neither of you are providing personal medical advice here.
That anything we talk about really is something people should just consider as information to talk with their medical provider about.
If these medications are used, are there things that we can do to minimize the potential of being floxed? And can things like magnesium or other nutrients decrease the risk of a bad outcome?
[00:39:01.06] Dr. Ghalili: Look, too many patients try to treat themselves, and sometimes they don’t know what they’re doing, and they just listen to 20 different people. And what works for one person may be detrimental to another because everyone has a different makeup; everyone was floxed differently.
Everyone took different medications with it, gadolinium contrast, right? Like you start moving that around by doing certain things, you can have severe damage, you cannot feel good for a couple of days. So that’s why no two people are the same with this, and no two people should ever be treated the same. But some tips, and I can’t give any medical advice specifically.
But I would think if it’s chelating magnesium out of your cells, that’s going to be very important mineral that you’re going to replenish in your body. Obviously, doing that in a safe manner and doing it the right way. But some patient’s even taking magnesium or they take like a bath with magnesium, they don’t feel well.
They’re detoxing; there’s so much going on with it that it has to be done differently for each person. So it’s very hard to say like I would say if you took magnesium with Cipro at the same time, you’re likely going to lower your risk of being floxed because then you don’t have that damage happening; you have something to offset the chelation part. That makes sense.
[00:40:19.17] Scott: And then I’ve read things like NAC or alpha-lipoic acid could potentially be helpful as well with dealing with the aldehyde issue that you mentioned. Is that something that you’ve seen benefit some people, Jason?
[00:40:30.21] Jason S.: Yes, I have. And there’s a study out of Poland where they had used Mitoq and some minerals to offset some of the gate leakage and the mitochondria. And NAC was a big proponent of that study.
And it seems to reduce the implications to the mitochondria, so I think it would be an effective strategy if you had to use these drugs. But first thing I would do is try not to take them, look for an alternative.
[00:40:54.16] Scott: So let’s talk about the mitochondria, this is going to be kind of a longer question, and then I’ll let you guys just run with it. But can supporting the mitochondria help once someone has been floxed? Is it too late at that point if we think about common mitochondrial supports like PQQ or Coq10 or various NAD molecules or precursors to NAD are very popular in the conversation today?
What are some of the mitochondrial supports that have helped people? And then extending on that in the whole mitochondrial arena, we have Dr. Bob Naviaux’s Cell Danger Response where ATP is actually the danger signal that shifts the body into this hypometabolic protective state, and you really want to then resolve the underlying infection or toxin or so on before you really start aggressively supporting mitochondria. So is there a timing aspect here that’s important as well relative to incorporating mitochondrial support in those people who have fluoroquinolone toxicity?
[00:41:53.23] Dr. Ghalili: Yes. So I think as soon as possible to get treated because you don’t want to end up like these patients five years down ten years down the road just dealing with issues. So I think getting it early on to prevent worsening is usually you see a downhill decline for the first maybe three to six months, and then a patient plateaus and then can slowly start getting better.
Many patients do get better on their own, and that’s always possible. But then you do have your, to me, it’s not worth the risk of knowing I’m going to end up like that, maybe one year or two years having issues, I’ll just personally get a treated asap. Look supplements. They’re different, like Mitoq, for example, that was brought up earlier.
I’ve seen that damage patients. I take it myself, and my tendons and muscles like don’t do well with it. I took PQQ early on, and I feel like you need to have healthy mitochondria first to take some of these supplements. Things like…NAD, like hey, some patients do absolutely, they don’t do well with it. I think it leads to a histamine response in some patients; they don’t do well, they don’t tolerate it.
And there’s a lot of things that I feel you need to have your mitochondria get healthy first before you start implementing and doing it slowly. And knowing what’s causing a side effect for you versus what’s getting you better. So it needs to be done in a, it’s very hard to do this on your own, you need someone kind of coaching you and guiding you along the way.
And many people kind of just try to take a bunch of things they may be damaging themselves. So it’s very important to research and do this in a slow way with guided help, and that’s going to be the best way to recover.
[00:43:30.28] Scott: So you mentioned that we need to get the mitochondria healthy before we start using things like PQQ or Mitoq, for example.
What are some of the things that would be keeping the mitochondria from being healthy or things that we would be thinking about to improve the health of the mitochondria before we started using some of these supportive interventions?
[00:43:50.25] Dr. Ghalili: Yes. So I mean you get toxic aldehyde formation, you get damage to the cells. You get this mitochondrial leakage, in my opinion, leading to this sort of damage. So it’s really doing things in a slow stepwise approach; you brought up magnesium earlier, right? Let’s get the cells what they need. Let’s get the minerals that they need first before we start aggressively going and treating the mitochondria.
Does that make sense? Let’s make sure we don’t have any other underlying issues going on. By like are we dealing with anything else other than this toxicity? That’s important first. Because you might need to take care of that before taking care of this. Are we on an antidepressant right now? Okay.
Well, there’s no point in going and treating you heavily right now because we got to get you off this fluoridated medication. You keep putting fluoride in your body; you keep taking ibuprofen every day. How do you expect to get better?
How do you expect to then take these mitochondrial supportive supplements and start seeing improvement when you’re just damaging the cells every day. So it’s a lifestyle, diet, avoiding exposure to these toxins that can be worsening your mitochondrial health, that’s first.
[00:45:02.03] Scott: So the correlation that’s coming to mind, and you can correct me if this doesn’t make sense. But the correlation that’s coming to mind here is in the mast cell activation and histamine and tolerance arena, we can take mast cell stabilizers, and we can take antihistamines.
But the reality is we need to find the underlying triggers for the mast cell activation. Look at the mold, look at the EMF exposure, look at the parasites, all of those kinds of things in order to have longer-term resolution of the problem.
And so the way I’m thinking of now PQQ and Coq10 and so on is kind of like the mast cell stabilizers. But we don’t want to jump there without getting at the underlying root causes or triggers first.
[00:45:41.22] Dr. Ghalili: Exactly.
[00:45:42.24] Scott: Okay, beautiful. You mentioned the toxicity aspect of these medications, is there an aspect of detoxification that can still be helpful? I’ve seen people providing things like homeopathic Levaquin, for example, with the idea of detoxifying the original trigger.
There are certainly conversations around detoxifying fluoride that we know we get exposed to from these medications. Could something like iodine, for example, be helpful in some people to reduce the fluoride burden that’s in their system?
[00:46:14.12] Dr. Ghalili: I’m not familiar with the homeopathic Levaquin, with the mechanism of how that works. But I’ll give you my two cents; once the drug does the damage, it does the damage. I mean, we know about the DNA adduct formation, the aldehydes, the free radical damage.
It’s like the damage has already been done; does that make sense? Like you completely dried that prune, well okay, what are you going to do? Like, inject water in it. It’s already kind of dried out; it’s not just to respond and just come back to life. So I don’t think there’s a way to necessarily take a pill to just say okay, we’re going to reverse the damage that’s been done.
It’s now our mitochondria has been damaged; we have this oxidative stress and free radical damage and all the other things going on. How do we help heal the nervous system? How do we heal the musculoskeletal system? So I take a different approach with that. When it comes to iodine, now, yes, studies show iodine can bind fluoride.
But we don’t know how much is actually being excreted. Also, with iodine, we have to be careful; too much iodine hyperthyroidism this needs to be done in a careful way where you’re not overdoing something.
But yes, studies do show that iodine can help pushing fluoride out. But the point I’m trying to make is the damage has already been done. So let’s get that fluoride out, so then we can use our mitochondrial support and go full force.
[00:47:39.06] Scott: You have lectured about antibiotics and the resulting increase in intestinal hyperpermeability or leaky gut, that can be particularly bad with fluoroquinolones, that Levaquin can negatively impact our microbiome as well.
And if that microbiome is impacted, that leads to increased food allergies and sensitivities. Can something like a focus on leaky gut or using tools like maybe colostrum, for example, that can help with that intestinal hyperpermeability. Can that be helpful in this realm?
[00:48:10.21] Dr. Ghalili: Yes, so we know leaky gut is proven that antibiotics can lead to leaky gut. And what it does is it blocks that, kind of opens up the zonulin channel. Zonulin closes the gap in your gut, and it decreases the permeability layer in that gut.
So certain foods you eat can cross that gut barrier, and then you get an autoimmune reaction, leading to inflammation, possibly mast cell, and histamine response. Colostrum, I’ve lectured, can help with that intestinal permeability, and we know in order to heal the brain, you have to heal the gut. Everything really starts in the gut, so healing that gut is key toward healing the whole body.
And we know that there’s a study performed that showed colostrum produce the stool concentration of zonulin. So there’s more zonulin now in the gut lining and not excreted through the stool. It was done in 2017 in Nutrients magazine.
[00:49:07.05] Scott: How much of a role does supporting the broader microbiome have in fluoroquinolone toxicity? And then are there specific organisms that maybe we need to focus on putting back into the body to improve the microbiome?
[00:49:20.14] Dr. Ghalili: I think it’s like an AK-47; it just kills everything. And then that’s how you get Candida overgrowth and fungal overgrowth in the body as well. And then what ends up happening? You get this fungal overgrowth, and you brought this up.
Scott, earlier, you brought up Diflucan number one go-to. So you’ve been floxed, you kill your normal gut bacteria. They throw Diflucan at you; then you’re ten times worse. Triple fluoride molecule. So it’s important to just get it all back. I can’t recommend, but high-dose probiotics may be beneficial because you got to rebuild that normal gut bacteria that you just lost.
[00:49:55.12] Jason S.: I can add Oxalobacter formigenes is like the most apparent strain of bacteria in the gut that gets hit. Pretty much 9 out of 10 people that take a fluoroquinolone have a problem with oxalate foods at some point in their life after they take these antibiotics.
[00:50:10.20] Scott: So that’s interesting because I’ve come across that; in fact, I talked about that on a previous podcast on oxalates. And one of the challenges was it wasn’t readily available in the U.S. So, Jason, is there a way to get that supplementally for people in the U.S that are dealing with fluoroquinolone toxicity or oxalate-related issues?
[00:50:30.00] Jason S.: Yes. So I’ve actually self-experimented with trying to rebuild that specific bacterial strain in my microbiome, and I found a company in India called Oxalo, and there’s also another one in Sweden that’s almost ready to come out with their OxThera I think it’s called, just to replenish that oxalobacter strain in the gut.
But for me, I still have long-lasting symptoms of when I eat almonds or spinach or sweet potatoes; I’ll get joint pain. And it feels like I have almost a glass on my skin sometimes when I have too many oxalate foods, and it’s literally because that fluoroquinolones are proven to reduce or eliminate that population in your microbiome.
[00:51:06.18] Scott: Yes. And it’s interesting the conversation we were having with you specifically earlier about the mold exposure because that can then be a producer of oxalates in the body as well. And so that’s another tie-in this whole conversation around oxalates and mold illness.
Let’s talk a little bit about collagen; so have you seen patients benefiting from taking supplemental collagen or maybe even from detoxification of glyphosate, which we know can predispose us to having weaker collagen?
[00:51:36.16] Dr. Ghalili: Well, we’re all exposed to glyphosate. You know Monsanto runs America, and many of the foods we have glyphosate in them. GMOs is really hard to avoid. And yes, that can reduce collagen. It’s hard to say because we don’t just treat patients with hairs here. Just take collagen.
We do like a full, well-rounded customized approach with multiple different avenues to try to attack this. So I don’t really have a study to show if just collagen by itself is helping. But I would say, in theory, giving collagen well; if we know we’re not able to produce collagen properly, then potentially taking it may be of benefit to some people.
But some aren’t damaged musculoskeletally, they’re fine, they could run, they could function, they can work out, they have neurological damage, right? So I want that patient having to take collagen every day and being annoying about it. Not as much as I would someone who’s having trouble with tendons and muscles, right?
[00:52:34.17] Scott: The macrophages can be in either an M1 type or an M2 type. The M2 type macrophages being able to increase collagen production, remodeling, regeneration, angiogenesis being really supportive.
Are there ways that we can shift our macrophages from that M1 type to the more beneficial M2 type?
[00:52:56.07] Dr. Ghalili: Yes. So one way that we do that here is we use adipose stem cell therapy. Where we know that adipose stem cells can shift the mesenchymal, the mesenchymal stem cells shift from M1 to M2.
M1 is a pro-inflammatory type, M2 is the anti-inflammatory macrophage. So you can get a TGF beta production, beta cell production. Increasing collagen production, which we need angiogenesis which is a formation of new blood vessels, right? Then we get more oxygen and more minerals to places we need, and ultimately cell regeneration.
[00:53:28.13] Scott: Talking then about minerals leads me to the question around IV nutrient therapies. In this patient population, have you seen IV nutrient therapies with minerals and other materials being potentially helpful for people that have been floxed?
[00:53:44.08] Dr. Ghalili: Yes, so these need to be done very carefully. We have patients going to nurses and different clinics who just offer IV therapy, and it’s like a one-size-fits-all. But I mean, you are floxed, so it’s different. Certain things need higher doses, so what you’re getting in some clinics, potentially they could put ingredients in there that could be potentially harmful to some patients. Some patients that may not be able to tolerate some of the ingredients in there.
So I’m a firm believer that these need to be customized for each individual patient depending on their history, physical exam, and what they’re exactly looking for. But again, some patients can take some certain type of B vitamins, for example, not feel well after; neuropathy can get worse with certain things.
So I like to specifically custom tailor for each patient. That’s why I think anyone who has chronic illness and is sick because if you could just go somewhere and just get an IV and everyone would feel better, no one would be sick. So it has to be done per patient as a customized approach, and that’s the only way that I’ve ever seen results.
[00:54:48.15] Scott: Is there a role for hormone replacement or bioidentical hormone replacement? If we look at things like estrogen or progesterone or testosterone. Can any of these things help to reverse or mitigate the damage from these fluoroquinolones?
[00:55:04.09] Dr. Ghalili: Yes, so that’s a great question. They’re not necessarily mitigating the damage, but we know the fluoroquinolones affect the hormone levels. Okay, so in my opinion, bind to that receptor, we need to reduce hormone production.
Males, the majority of males, I would say 99% of the males who come in have low free testosterone levels, low total testosterone, high sex hormone-binding globulin levels. By supplementing testosterone, and you’re not reversing the fluoroquinolone toxicity, but you’re helping, depending on what the labs are.
It’s things you may want to look at it can potentially help you increase muscle mass help you increase tendon strength. But it just helps the process get going faster, gives you strength, helps you with your energy, right? So whether you’re floxed or not, having a low testosterone level, for example, if you replace that safely, you’re going to feel better.
The majority of people will feel great. So that’s why it can be incorporated because we know the hormone levels are changed. Estrogen, progesterone, having females potentially get on hormone replacement, it may be beneficial to them. But it’s a case-by-case basis, right? Hormone replacement we know sometimes can increase the risk of blood clots, right? So you have to be very careful with how you do this.
[00:56:15.06] Scott: If we come back to the tendon conversation, and there are those cases where there’s scarring or adhesion or fibrosis.
Are there certain things like extracorporeal shockwave therapy or maybe Gua sha or Graston? How can we approach the adhesion or fibrosis, or scarring aspect of the tendon injury?
[00:56:39.23] Dr. Ghalili: Oh, that’s so tough. I haven’t used the extracorporeal shockwave therapy in my office personally. I would think doing it too early can potentially lead to damage. So it might not be something you’d want to do in an acute phase. But again, it’s not something I’ve implemented or can comment on.
[00:56:57.10] Scott: Is there anything that you do consider therapeutically for the fibrosis aspect of this? Even aside from the shockwave therapy?
[00:57:06.23] Dr. Ghalili: Yes. I would say if anything can go in and potentially help with that, couple times should be stem cell therapy. That’s new and cutting edge that can go in. Mineral nutrient replacement, right diet lifestyle that all helps as well.
But I don’t necessarily have anything more specifically. Because we don’t, we don’t necessarily know if it’s fibrosis, right? We don’t necessarily know. Because well, if you have tears, you can get scar tissue there, okay. And that could lead to limitations.
But if you don’t have a tear, we don’t necessarily know if we’re dealing with fibrotic scar tissue there. We might just be dealing with kind of damaged mitochondria. Because when you get an MRI, like 99% of patients who have MRIs of their joints wherever their muscles, tendons it usually shows up as normal, and they don’t really note any fibrotic changes in these MRIs and scans. And that’s what’s making us hypothesize that this is all due to mitochondrial damage and toxicity.
[00:58:06.12] Scott: We talked earlier about the small fiber neuropathy that can be seen in this condition, that is common in Lyme disease as well. Some people will use IVIG to help with repairing that damage. I’m wondering if you’ve seen IVIG as a potentially helpful tool in people that have been floxed.
[00:58:26.15] Dr. Ghalili: So IVIG interferes with cytokine production, and it alters maturation of T and B cells. I personally have not used it for this condition, but I don’t see how it can benefit, because as I said, your body is not attacking itself with fluoroquino toxicity; the damage has already been done.
IVIG is used for like an immune response. I just don’t see any logic in it being beneficial. I’ve even had patients harmed by it who have tried IVIG because the doctor had no idea what to do and was just let’s just try something, and it’s made them worse. So personally, I can’t get medical advice, but I wouldn’t do that for myself if I was floxed.
[00:59:09.09] Scott: From the mitochondrial perspective, what are your thoughts on the use of red light therapy or photobiomodulation to help provide that light and photonic support that then can help the mitochondria. Have you seen red light therapy as a helpful tool?
[00:59:25.13] Dr. Ghalili: Yes. So I love low-level laser light therapy or led therapy. It has great functions in terms of increasing blood flow by increasing nitric oxide. It can reduce inflammation in the body, now that we’re dealing with inflammation.
It can increase ATP production within the cells, and studies have shown it can increase stem cells from the bone marrow. So I think it’s a great additive to have, and I don’t see it doing any harm.
[00:59:52.04] Scott: Let’s talk a little bit about ozone therapy or prolozone. Is that something that you think could have a localized benefit for people that have been floxed? And could something like even hyperbaric oxygen therapy, for example, could that be helpful in this community?
[01:00:08.28] Dr. Ghalili: Yes. So I don’t really implement these strategies for floxed patients, but hyperbaric oxygen sure, getting high amounts of oxygen in the system, there’s nothing wrong with that. And if the patients can tolerate that, that’s great.
But I don’t see it being a long-term effect. Like Dr. Ordon from the doctor’s show, who we treated had about 20 or so hyperbaric oxygen treatments done; it didn’t do anything for him for the fluoroquinolone toxicity.
Sure it may give you a little energy; you have more oxygen, you’re more alert, you feel better. But at the end of the day, it’s not reversing that fluoroquinolone toxicity. Is it great to get oxygen to the tendons? Yes. Don’t get me wrong, but that’s not the end all be all.
Ozone therapy is O3; ozone is O3. It can actually initially potentially increase oxidative stress mildly, increase the lipid peroxidation in the cells. So it might be something to implement once the body’s healthy.
But it’s not something I implement in the beginning phases. Some patients don’t react and respond to it well. So it goes on a case-by-case basis.
[01:01:14.23] Scott: If we look at the application of frequency-based tools, let’s say pulsed electromagnetic field therapy, for example, that can increase circulation, increase oxygenation, or even tools like Frequency Specific Microcurrent from Dr. Carolyn McMakin for example.
Have you found either of these tools as helpful interventions?
[01:01:34.13] Dr. Ghalili: Yes, So PEMF increases blood flow, increases the nitric oxide to make cyclic GMP, and that can create growth factors, vascular endothelial growth factors. And TNF alpha for increasing collagen.
So I’ve used it before in the past, but again, this is one of those things where if you use too early, you might feel worse before you feel better. That’s why it’s so tricky with this. And how to use it. But PEMF, like for a normal person, PEMF is amazing. Like who hasn’t been floxed, no issues. They’ll feel a lot of energy and benefit from it.
Also, a lot of people use too high of a setting initially at first without building up to it. So as long as you do it slowly and safely and see if it works for you, go ahead and try it. But again, I don’t think that’s like the end-all-be-all of reversing the condition just by using PEMF.
I’ve used the BEMER mat before, but I had a patient who uses it as well who use PEMF too early on, and they’ve had like severe side effects. I think it’s safer to use like later on, not in the acute phase but in the chronic phase. I can see it providing some benefit.
[01:02:45.12] Scott: In the regenerative medicine realm, some in the Lyme community have explored stem cell therapies. You’ve talked about that.
I personally have had PRP-based injections for different growth factors and things when I had a shoulder injury, for example. Are there tools in the regenerative medicine realm that are emerging that you think have potential for the Floxie community?
[01:03:09.19] Dr. Ghalili: Yes, definitely. I had adipose stem cell therapy performed myself, so that’s why I highly believe in it. I saw the difference it did for me, what it’s doing for other patients. I think it’s very important, but I also think it’s important to optimize getting the body optimized first, diet lifestyle, avoiding things like fluoride like we discussed earlier.
I’m getting the nutrients we discussed about earlier in and then potentially having stem cell therapy perform. It’s experimental; it’s under an IRB-approved protocol. Getting those cells, shifting the M1 macrophage to the M2 to reduce inflammation, increase vascular endothelial growth factors, increase angiogenesis.
That’s what we’re going for with the stems. Stem cells recruit growth factors in cytokines areas of injury based on the studies in the data, and our network, cell surgical network has had, I believe we’re at the whole network as a whole is about 13,000 procedures performed.
All the data is on their website; pretty much have seen great results from it. But it’s optional for a patient; not every single patient has it done. So I like it; I think it’s great for people. And whether you’re healthy, you’ve got fluoroquinolone toxicity. I think it’s something that could benefit you because it’s going to have an anti-aging effect as well.
[01:04:32.03] Scott: With treatment of this condition, what is the prognosis for patients? Does the damage fully heal? Can the mitochondrial function be restored? Or is this a condition that is generally managed over the long term?
[01:04:45.15] Dr. Ghalili: I’ve seen patients make full recoveries. I mean, personally, myself made 100% recovery. We have patients who make 50% recoveries. I’ve seen people who just, no matter what you do for them.
It could be a psychological issue component as well due to that GABA receptor that we discussed potentially being displaced and having like high levels of anxiety, and just being negative. I’ve had patients say, oh well, I don’t feel any difference or changed; I’ve been living like this for ten years.
Some people don’t even know what normal was because they’ve been dealing with us so long, and it’s so unfortunate that they don’t even remember who they were before. And those are the saddest cases I see. I don’t really have a number to say because it’s per patient.
So someone might say I feel 90% better. But to that other person, feeling 90% better might be I only feel 10% better.
[01:05:36.21] Jason S.: So I feel once you go through this traumatic experience of being normal, and then getting hit by a prescription medication that you thought was safe, that you trusted your doctor to give you and you believed was going to help you.
And this, like psychological trauma that you go through, does have some PTSD, in my opinion. It lingers, right? This is an event that happened to you. It’s not a part of you per se, but I feel a lot of people do heal, and they get some semblance of their life back.
That they’re more humble people, I would say, and more well-versed in their body and supplementation diet. And just creating this space around them, that’s about healing and being well after this antibiotic shook their life so tragically for sure. But it does get better.
[01:06:28.16] Scott: I would say that this community, the Floxie community is largely underserved, that it’s difficult to find people that know how to address this condition, that can provide some support. So what are some resources that we can recommend to provide support for people that are dealing with this condition?
[01:06:46.11] Dr. Ghalili: Jason knows FloxieHope.com, a lot of great information there for patients.
[01:06:52.10] Jason S.: Yes. I feel like FloxieHope. It’s a one-stop, right? You can go there; you can get hope; you can get inspiration by people that have healed. There are tons of good blog articles on the mechanisms of action, connecting the dots for people that there’s a place where you can talk to other floxies.
So it’s been around for over a decade, and it’s helped thousands. I mean, thousands and thousands of people visit the site every month tragically because it means that there are more people getting affected by these drugs. But there’s a wealth of information to give people hope, inspiration, and guidance.
[01:07:28.07] Scott: And we’ll put the links to FloxieHope as well as to Dr. Ghalili’s site as well in the show notes. I know one of the things that I was really excited about was seeing some of the videos on Dr. Ghalili’s site of people where you could actually see them before and after treatment, and how they were moving and their limitations largely being significantly improved.
And so, I would urge people to take a look at that as well. My last question is the same for every guest, and that is what are some of the key things you do on a daily basis in support of your own health?
[01:07:58.06] Scott: Oh yes, great question. I’m personally plant-based; I’m a vegan. I want to avoid all meat that have steroids or antibiotics in them. I feel like I’ll never have them again. I avoid fluoride at all costs. I’m organic.
Make sure I try to do non-GMO. Exercise, work out all the time, and yes, I drink a reverse osmosis water; it doesn’t have any fluoride in it. And I maintain myself with IVs and different treatments I do. Whatever I can to just help myself be optimized and be on my full potential.
[01:08:28.19] Jason S.: For me, my top three things that I do every day that I believe are important and really getting me my fullest potential in my own health journey is meditation, breathwork, and red light therapy. I make time for that every day, and it’s been some of the biggest changes in my health for sure, just using those every day.
[01:08:53.00] Scott: Very nice. This has been such a great conversation; I learned a lot. I know people are going to benefit from hearing your experience Dr. Mark with treating the condition.
And Jason, your personal experience, and all the work that you’re doing to be a patient advocate and really help minimize, both of you really helping to minimize the suffering of others. I want to thank you both for spending your time today and being so generous in sharing this information. So thanks for being here.
[01:09:17.25] Dr. Ghalili: Thank you so much for having us. What you’re doing is incredible, really raising awareness. So thank you for what you do and spreading your voice, and using your platform to do good for people.
[01:09:29.00] To learn more about today’s guests, visit Dr. Mark Ghalili at RegenerativeMedicineLA.com. That’s RegenerativeMedicineLA.com. RegenerativeMedicineLA.com, or find Jason Sousa and the Floxie Hope community at FloxieHope.com. That’s Floxie, F-L-O-X-I-EHope.com. FloxieHope.com.
[01:09:56.28] Thanks for listening to today’s episode. If you’re enjoying the show, please leave a positive rating or review, as doing so will help the show reach a broader audience. To follow me on Facebook, Instagram, Twitter, or MeWe, you can find me there as better health guy.
To support the show, please visit BetterGealthGuy.com/donate. To be added to my newsletter, please visit BetterGealthGuy.com/newsletters. This and other shows can be found on YouTube, Apple Podcasts, Google Podcasts, Stitcher, and Spotify.
[01:10:31.26] Thanks for listening to this BetterHealthGuy Blogcast with Scott, your Better Health Guy. To check out additional shows and learn more about Scott’s personal journey to better health, please visit BetterHealthGuy.com.











… [Trackback]
[…] Read More on on that Topic: floxiehope.com/floxie-hope-on-the-better-health-guy-podcast/ […]
… [Trackback]
[…] Here you will find 46370 more Information on that Topic: floxiehope.com/floxie-hope-on-the-better-health-guy-podcast/ […]
… [Trackback]
[…] Info on that Topic: floxiehope.com/floxie-hope-on-the-better-health-guy-podcast/ […]
… [Trackback]
[…] Read More Information here to that Topic: floxiehope.com/floxie-hope-on-the-better-health-guy-podcast/ […]
… [Trackback]
[…] Here you will find 30411 additional Info to that Topic: floxiehope.com/floxie-hope-on-the-better-health-guy-podcast/ […]
… [Trackback]
[…] Read More on that Topic: floxiehope.com/floxie-hope-on-the-better-health-guy-podcast/ […]
… [Trackback]
[…] There you will find 73359 more Info to that Topic: floxiehope.com/floxie-hope-on-the-better-health-guy-podcast/ […]