GABA “is the chief inhibitory neurotransmitter in the mammalian central nervous system. Its principal role is reducing neuronal excitability throughout the nervous system. In humans, GABA is also directly responsible for the regulation of muscle tone” (source). Fluoroquinolones “are known to non-competitively inhibit the activity of the neurotransmitter, GABA, thus decreasing the activation threshold needed for that neuron to generate an impulse.” (source, source, source) Fluoroquinolones have also been shown to have similar effects on GABA neurotransmitters as benzodiazepine withdrawal (source).
The effects of fluoroquinolones on GABA-A neurotransmitters are the exact opposite of the effects of benzodiazepines, and, on a neurotransmitter level, they are the same as the effects of benzodiazepine withdrawal.
Symptoms of benzodiazepine withdrawal, AND fluoroquinolone toxicity, include:
- sleep disturbances
- irritability
- increased tension and anxiety
- panic attacks
- tremors
- difficulty with concentration
- confusion and cognitive difficulty
- memory problems
- nausea
- heart palpitations
- headaches
- muscular pain and stiffness
- psychosis
And many other symptoms.
Both fluoroquinolone toxicity and benzodiazepine withdrawal are multi-symptom, chronic illnesses, for which there is no cure, and, despite significant research into both, the severity and complexity of both SYNDROMES is rarely acknowledged.
The following article does a brilliant job of connecting fluoroquinolone toxicity (syndrome) and benzodiazepine withdrawal (syndrome), and it gives a thorough explanation as to why people who have gone through benzodiazepine withdrawal should NEVER be prescribed fluoroquinolones. The article was originally published on the Benzodiazepine Information Coalition web site, www.benzoinfo.com, in October, 2016. It was written by Brad Verret, and I am grateful to him for the wonderful article.
Tragically, Brad Verret has passed away. I asked the editor of benzoinfo.com if I could re-publish it on floxiehope.com, and she said yes and noted that, “Brad wrote his articles to help as many people as possible. His intentions were to sound the alarm for benzodiazepine affected people to avoid that awful class of antibiotics, and he would have been pleased to help floxies avoid getting benzodiazepine injured.” She also noted that Brad was kind and smart and that he is missed dearly. I hope that his loved-ones see the use of his wonderful article as a tribute. Brad synthesized and interpreted the data about the effects of fluroquinolones and benzodiazepines on GABA-A thoughtfully and insightfully. This is a wonderful article, and Brad’s work is greatly appreciated! Please share it (or this entire post) far and wide – thank you!!
Hidden Dangers of Fluoroquinolone Antibiotics in the Benzodiazepine-Dependent Population
By Brad Verret
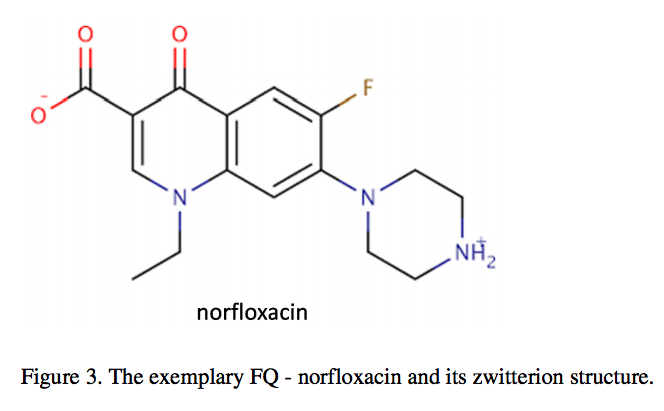
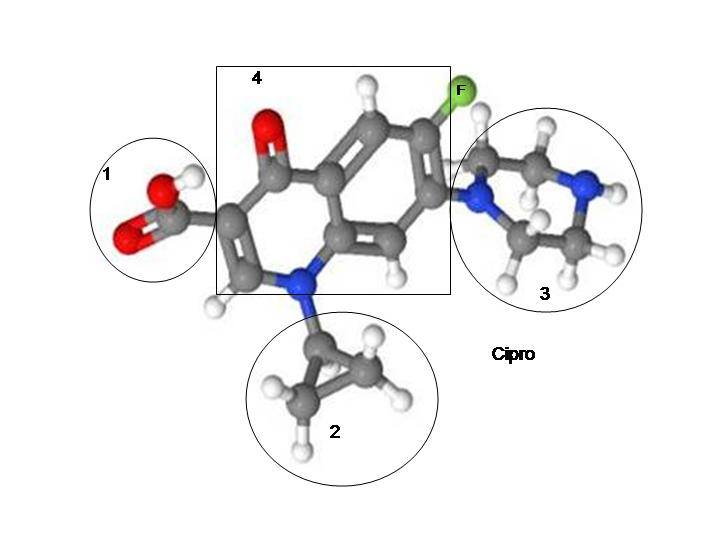
Whether it was for a sinus infection or bronchitis, most people have taken an antibiotic at some point in their lives. Antibiotics can be lifesaving medications but, like all other drugs, they come with risks. In particular, one specific class of antibiotic drugs called the fluoroquinolones carry serious risks that few people are aware of. In light of the growing epidemic of antibiotic resistance, each new generation of antibiotics has bolstered an enhanced degree of potency which can be viewed as both an asset and a liability. The fluoroquinolone class features a robust, broad-spectrum antibiotic effect and includes many popular drugs such as ciprofloxacin (Cipro), ofloxacin (Floxin), norfloxacin (Noroxin), levofloxacin (Levaquin), moxifloxacin (Avelox), and gemifloxacin (Factive).
Chemically speaking, the mechanism of action of the fluoroquinolones closely mirrors that of certain chemotherapy drugs, so it is rather unsettling that these powerful agents are sometimes prescribed for relatively benign infections that would probably resolve on their own or with a milder drug. One notable and unique risk of the fluoroquinolones is that, unlike most other antibiotics, they are neurologically active at commonly prescribed dosages. As an action secondary to their primary antimicrobial effect, they are capable of binding to certain receptors in the brain, spinal cord, and peripheral nervous system. The primary receptor type affected is the GABA-A receptor, which is the exact same receptor that benzodiazepines act on.[1]
When a fluoroquinolone binds to a GABA receptor, the result is the polar opposite of the effect of CNS depressants like benzodiazepines. Fluoroquinolones are antagonists of the GABA-A receptor, meaning that they prevent the binding of GABA and can displace other molecules bound to the receptor, such as benzodiazepines.[1] GABA is an inhibitory neurotransmitter and drugs which enhance its action, like benzodiazepines, cause sedation. The GABA receptor blockade caused by a fluoroquinolone results in a CNS stimulant effect, with neurological manifestations ranging from mild insomnia and agitation to hallucinations and seizures.[2] Anyone can suffer these side effects, but individuals prescribed benzodiazepines are notably much more prone to experiencing these adverse neuropsychiatric reactions.
The culprit is the GABA receptor downregulation imposed by benzodiazepine tolerance. When a benzodiazepine is given chronically (beyond 10 days) there are a series of downward compensatory mechanisms which seek to restore a neurological equilibrium in light of the overstimulation of GABA receptors by the drug. This results in GABA receptors becoming progressively less receptive to GABA over time following prolonged exposure to benzodiazepines.[3] Over time, the brain’s GABA-dependent systems are weakened and there is a heightened vulnerability to external influences which decrease the action of GABA.
A storm neural excitation ensues when a fluoroquinolone “unmasks” the GABA receptor downregulation associated with benzodiazepine tolerance. In addition, since they share the same target, fluoroquinolones are capable of competing with benzodiazepines for GABA receptor binding in a concentration-dependent manner. Studies have shown a complex interaction when a fluoroquinolone and a benzodiazepine are simultaneously bound to a GABA receptor. At high concentrations, fluoroquinolones are capable of displacing a portion of the benzodiazepine molecules bound to GABA receptors.[4]This displacement can precipitate an acute benzodiazepine withdrawal syndrome which is identical to that which would normally happen if an individual were to suddenly reduce their benzodiazepine dosage.
Imagine each GABA receptor as having a gas pedal and a brake pedal. The entire GABA receptor, with its imaginary gas and brake pedals, is anchored into the neuron whose pace it controls. GABA agonists like benzodiazepines act on the brake pedal and GABA antagonists like fluoroquinolones act on the gas pedal. When an agonist acts on the brake pedal, chloride ions flow through the receptor into the neuron. Chloride ions are like an electrostatic glue which slows the neuron down. When an antagonist acts on the gas pedal, the flow of chloride stops and the neuron speeds up.
When an agonist is present for a prolonged period of time, the brake pedal gradually becomes worn out. Additionally, the neuron will recruit chemical messengers to tune up the gas pedal so that the neuron can continue to move along at its desired pace. It might be a pace that provokes anxiety, but it is the precise pace which will allow the neuron to fulfill its purpose within the unique neural circuit it belongs to. After being chronically slowed down by benzodiazepines, neurons want to break free but are held back by the presence of the drug. They will progressively fight back harder and harder to overcome this pharmacological oppression. Fluoroquinolones unleash neurons from their chemical bondage by disengaging the brake and stepping on the gas pedal, causing a sort of neural short-circuit as the freed neurons begin to race out of control.
It has been shown that certain non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen are capable of enhancing the GABA receptor blockade cause by fluoroquinolones, potentiating their neurotoxicity and exacerbating their CNS side effects.[5] NSAIDs are frequently co-prescribed with fluoroquinolone antibiotics for painful infections like sinusitis and urinary tract infections. Adding further insult to injury, some fluoroquinolones including ciprofloxacin (Cipro) are inhibitors of the CYP1A2 liver enzyme which is responsible for metabolizing caffeine and other xanthine alkaloids found in coffee, tea, and chocolate.[6] This commonly results in an increased sensitivity to the stimulating effects of caffeine when ciprofloxacin is taken. Hence, it is hardly a surprise that coffee drinkers who are prescribed a benzodiazepine are at an even higher risk for fluoroquinolone-induced seizures and neuropsychiatric disturbances.
It is an unfortunate truth that many healthcare practitioners outside the realm of neuroscience are unaware of these lesser-known facts about fluoroquinolone antibiotics. The fluoroquinolone-caffeine interaction is well documented but the fluoroquinolone-benzodiazepine interaction is not currently recognized in any of the current web-based drug interaction cross checking systems commonly used by healthcare consumers. Most pharmacists are not aware of the issue either, and will readily dispense fluoroquinolone prescriptions to benzodiazepine-dependent patients. This interaction is not consistently recognized yet it very consistently gets benzodiazepine-tolerant individuals into deep trouble. Studies have found that benzodiazepine-dependent individuals frequently experience depression, anxiety, psychosis, paranoia, severe insomnia, paraesthesia, tinnitus, hypersensitivity to light and sound, tremors, seizures, and suicidal thoughts upon exposure to fluoroquinolone antibiotics.[7]
These symptoms are all consistent with acute benzodiazepine withdrawal syndrome. Furthermore, it may take several weeks or even months after discontinuing the fluoroquinolone for the affected individual to become symptom-free. This may be due to the long-term potentiation that occurs when excitatory glutamate-containing synapses are overstimulated by a deficit of GABA activity. Some individuals never return to their pre-fluoroquinolone state and they are commonly referred to as having been “floxed”. They are left with conditions including peripheral neuropathy, muscle weakness, cognitive dysfunction, new or worsened mental illness, and even paralysis which are all consistent with excitatory neurotoxicity (excitotoxicity) and brain damage.[8][9][10]
Taking all this into account, it is imperative that moving forward more healthcare professionals will become aware of and publicly acknowledge this dangerous interaction which has rendered normal, healthy people disabled. However, this alone is not enough. It is equally important that benzodiazepine-dependent individuals become aware of this interaction so that they can better advocate for themselves. It is well known that chronic benzodiazepine usage often creates chemical sensitivities which require the affected individuals to avoid a variety of foreign substances which most normal people can tolerate, and fluoroquinolones probably fall at the very top of that list.
All doctors should be aware that prescribing a fluoroquinolone to a benzodiazepine-dependent individual carries a serious risk for disability which could potentially be permanent. Fluoroquinolones should be contraindicated with chronic benzodiazepine exposure in nearly every scenario, including nonmedical benzodiazepine abuse. Clinicians should explore all alternatives before fluoroquinolones are considered. In rare cases where it has been determined that failing to administer a fluoroquinolone could result in death, benzodiazepine-dependent individuals should have their benzodiazepine dosages increased for the entire duration of fluoroquinolone therapy and until the drug is completely cleared from their system.












… [Trackback]
[…] Read More Information here to that Topic: floxiehope.com/fluoroquinolone-toxicity-mimics-benzodiazepine-withdrawal-beware/ […]
… [Trackback]
[…] Info to that Topic: floxiehope.com/fluoroquinolone-toxicity-mimics-benzodiazepine-withdrawal-beware/ […]
… [Trackback]
[…] There you can find 46732 additional Info on that Topic: floxiehope.com/fluoroquinolone-toxicity-mimics-benzodiazepine-withdrawal-beware/ […]
… [Trackback]
[…] Find More Info here to that Topic: floxiehope.com/fluoroquinolone-toxicity-mimics-benzodiazepine-withdrawal-beware/ […]
… [Trackback]
[…] Find More on that Topic: floxiehope.com/fluoroquinolone-toxicity-mimics-benzodiazepine-withdrawal-beware/ […]
… [Trackback]
[…] Find More here on that Topic: floxiehope.com/fluoroquinolone-toxicity-mimics-benzodiazepine-withdrawal-beware/ […]
… [Trackback]
[…] Info on that Topic: floxiehope.com/fluoroquinolone-toxicity-mimics-benzodiazepine-withdrawal-beware/ […]
… [Trackback]
[…] Find More here to that Topic: floxiehope.com/fluoroquinolone-toxicity-mimics-benzodiazepine-withdrawal-beware/ […]
… [Trackback]
[…] Here you can find 87386 more Info on that Topic: floxiehope.com/fluoroquinolone-toxicity-mimics-benzodiazepine-withdrawal-beware/ […]
… [Trackback]
[…] Find More Information here to that Topic: floxiehope.com/fluoroquinolone-toxicity-mimics-benzodiazepine-withdrawal-beware/ […]
… [Trackback]
[…] Read More on that Topic: floxiehope.com/fluoroquinolone-toxicity-mimics-benzodiazepine-withdrawal-beware/ […]
… [Trackback]
[…] Find More Info here on that Topic: floxiehope.com/fluoroquinolone-toxicity-mimics-benzodiazepine-withdrawal-beware/ […]
… [Trackback]
[…] Find More here to that Topic: floxiehope.com/fluoroquinolone-toxicity-mimics-benzodiazepine-withdrawal-beware/ […]
… [Trackback]
[…] Read More on that Topic: floxiehope.com/fluoroquinolone-toxicity-mimics-benzodiazepine-withdrawal-beware/ […]
… [Trackback]
[…] Info to that Topic: floxiehope.com/fluoroquinolone-toxicity-mimics-benzodiazepine-withdrawal-beware/ […]
… [Trackback]
[…] Information to that Topic: floxiehope.com/fluoroquinolone-toxicity-mimics-benzodiazepine-withdrawal-beware/ […]
… [Trackback]
[…] Read More Information here to that Topic: floxiehope.com/fluoroquinolone-toxicity-mimics-benzodiazepine-withdrawal-beware/ […]