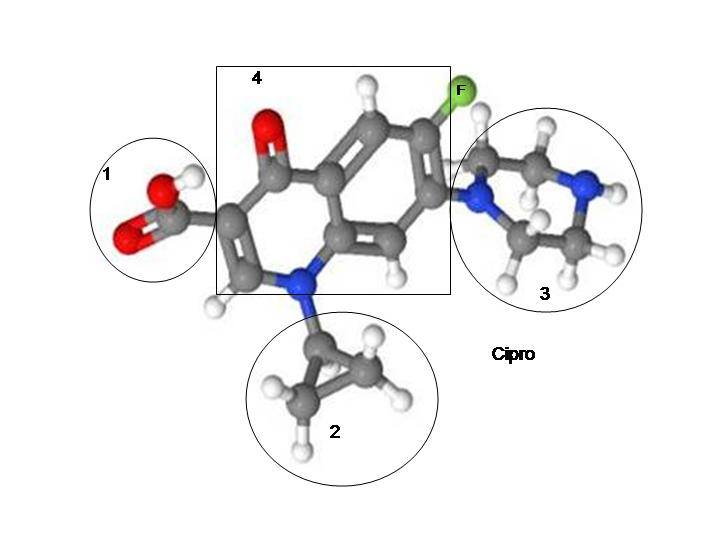
Several fluoroquinolones have been removed from the market because they caused acute toxicity and death. The fluoroquinolones that have been removed from the market are not terribly different from the ones that remain on the market in terms of damage done or damage mechanisms.
Here are some of the fluoroquinolones that have been removed from the market:
Omniflox/temafloxacin
In 1992 the fluoroquinolone antibiotic Omniflox/temifloxacin was removed from the US market after causing three deaths.
To note the removal from the market, the FDA released the following statement:
“The Food and Drug Administration today announced that Abbott Laboratories of Abbott Park, Ill., is voluntarily recalling the broad-spectrum anti-infective drug Omniflox (temafloxacin) tablets, and will halt all further distribution of the drug.
This action is being taken because of severe adverse events associated with the use of the drug that have been reported to the company and to FDA in the first three months of marketing.
Temafloxacin was approved in late January 1992 and marketed in mid-February. Since that time there have been approximately 50 reports of serious adverse reactions, including three deaths. There were several cases of severe low blood sugar, especially in very elderly patients with decreased kidney function. Among the severe reactions there were a number of cases of an unusual complex of adverse reactions consisting of hemolitic anemia (destruction of red blood cells) and other blood cell abnormalities.”
The fluoroquinolones that remain on the market also impair kidney function. From the 2013 Science Daily article, Risk of kidney disease doubled with use of fluoroquinolone antibiotics, “The risk of acute kidney disease is doubled for people taking oral fluoroquinolone antibiotics, according to a new study.” The article pointed out that the risk of acute kidney disease was increased for patients taking cipro/ciprofloxacin, levaquin/levofloxacin, avelox/moxifloxacin and floxin/ofloxacin – fluoroquinolones that remain on the market today.
The fluoroquinolones that remain on the market also cause blood-sugar abnormalities, including severe low blood sugar. A large 2013 study out of Taiwan looked at more than 78,000 patient records and found that, “The researchers found that patients with diabetes who had taken fluoroquinolone antibiotics had higher rates of both hyperglycemia and hypoglycemia compared with those who had taken macrolide antibiotics.” (source) Additionally, in the article, Fluoroquinolone antibiotics and type 2 diabetes mellitus, it is noted that, “Exposure to fluoroquinolone antibiotics is postulated as a risk factor for subsequent development of type 2 diabetes. It is hypothesized that fluoroquinolones induce an intracellular magnesium deficit that can lead to insulin resistance.”
Raxar/grepafloxacin
Raxar/grepafloxacin was removed from the worldwide market in 1999. The FDA withdrawal notice stated:
RAXAR is a fluoroquinolone antibiotic indicated for the treatment of infections caused by strains of bacteria susceptible to grepafloxacin in the following diseases: community-acquired pneumonia; acute bacterial exacerbations of chronic bronchitis; uncomplicated gonorrhea (urethral in males and endocervical and rectal in females); non-gonococcal urethritis and cervicitis.
Glaxo Wellcome has recently concluded an extensive review of the safety of RAXAR and determined that due to an effect of RAXAR on cardiac repolarization, manifested as QT interval prolongation on the electrocardiogram (ECG), some patients may be at risk of a very rare but serious ventricular arrhythmia known as torsade de pointes when treated with the product.
The warning label for Levaquin/levofloxacin (and the other fluoroquinolones that remain on the market) notes that:
“Prolongation of the QT interval and isolated cases of torsade de pointes have been reported. Avoid use in patients with known prolongation, those with hypokalemia, and with other drugs that prolong the QT interval.”
Additionally, a study entitled “Azithromycin and Levofloxacin Use and Increased Risk of Cardiac Arrhythmia and Death” compared the risk of cardiac arrhythmia for U.S. Veterans taking amoxicillin, azithromycin and levofloxacin. The study concluded that:
“Compared with amoxicillin, azithromycin resulted in a statistically significant increase in mortality and arrhythmia risks on days 1 to 5, but not 6 to 10. Levofloxacin, which was predominantly dispensed for a minimum of 10 days, resulted in an increased risk throughout the 10-day period.”
Just like Raxar/grepafloxacin, the fluoroquinolones that are still on the market prolong the QT interval and cause torsade de pointes, which can lead to arrhythmia and death.
Zagam/sparfloxacin
Zagam/Sparfloxacin was also removed from the market because it caused QT interval prolongation.
Zagam/Sparfloxacin also caused incidents of Stevens Johnson Syndrome:
“When a patient using Zagam develops SJS or TEN after taking the fluoroquinolone antibiotic treatment, the individual’s topmost skin cells die and fall off. This leaves the deeper layers exposed and unprotected, making it likely for a patient to experience infection and scarring. The sensitive mucous membrane also becomes exposed when the upper layer of skin sloughs off, and may be prone to blistering.” (source)
Trovan/trovafloxacin
Trovan/Trovafloxacin was removed from the market because of its high potential for inducing serious, sometimes fatal liver damage (hepatotoxicity). The wiki entry for Trovafloxacin notes that:
In June 1999 the U.S. Food and Drug Administration advised doctors to limit the prescription of Trovan after it had been found “strongly associated” with 14 cases of acute liver failure and six deaths. The FDA had received over 100 reports of liver problems in people taking Trovan, which was at that time being prescribed at a rate of 300,000 patients per month in the United States. Two days later the Committee for Proprietary Medicinal Products recommended to the European Commission that marketing approval of Trovan be suspended for a year.
One of the best articles about the hepatotoxicity of Trovan/Trovofloxacin is Trovafloxacin, a fluoroquinolone antibiotic with hepatotoxic potential, causes mitochondrial peroxynitrite stress in a mouse model of underlying mitochondrial dysfunction. The article, Mechanisms of Pathogenesis in Drug Hepatotoxicity Putting the Stress on Mitochondria, by some of the same authors, is also enlightening. Liver damage, mitochondrial damage, and ROS overload/oxidative stress are all intricately connected. I highly recommend that you read the two articles linked to (but, man, they’re both really difficult articles). I suspect that both articles hold many of the keys to understanding all fluoroquinolone toxicity reactions. In the post, Article Breakdown – “Mechanisms of Pathogenesis in Drug Hepatotoxicity Putting the Stress on Mitochondria,” I go over some of the implications Mechanisms of Pathogenesis in Drug Hepatotoxicity Putting the Stress on Mitochondria has for floxies.
Interestingly, Trovan/Trovafloxacin has another area of shady history. In Kano, Nigeria, it was used in an improperly conducted trial on children with meningitis. Per the wiki entry for Trovafloxacin:
In 1996, during a meningitis epidemic in Kano, Nigeria, the drug was administered to approximately 200 [3] infected children. Eleven children died in the trial: five after taking Trovan and six after taking an older antibiotic used for comparison in the clinical trial. Others suffered blindness, deafness and brain damage, common sequalae of meningitis that have not been seen in patients treated with trovafloxacin for other infection types.[4][5][6] An investigation by the Washington Post concluded that Pfizer had administered the drug as part of an illegal clinical trial without authorization from the Nigerian government or consent from the children’s parents.[7] The case came to light in December 2000 as the result of an investigation by The Washington Post, and sparked significant public outcry. The most serious error was the falsification and backdating of an ethics approval leader by the lead investigator of the trial, Dr. Abdulhamid Isa Dutse. Dr. Dutse is now the chief medical officer of Aminu Kano Teaching Hospital. The result of the trial was that children treated with oral trovafloxacin had a 5% (5/100) mortality rate compared to a 6% (6/100) mortality rate with intramuscular ceftriaxone.
Between 2002 and 2005 the victims of the Trovan tests in Nigeria filed a series of unsuccessful lawsuits in the United States. However, in January 2009, the United States Court of Appeals for the Second Circuit ruled that the Nigerian victims and their families were entitled to bring suit against Pfizer in the United States under the Alien Tort Statute. A US$75 million settlement with the State of Kano was reached July 30, 2009.[8] Additionally two lawsuits also remain pending in New York, United States.[8] According to Wikileaked US embassy cables, Pfizer’s country manager admitted that “Pfizer had hired investigators to uncover corruption links to federal attorney general Michael Aondoakaa to expose him and put pressure on him to drop the federal cases.”[9]
Additional information about the Kano trial can be found in The Guardian article, Pfizer pays out to Nigerian families of meningitis drug trial victims.
Tequin/gatifloxacin
Tequin/Gatifloxacin was pulled from the market because it caused severe blood sugar reactions such as hyperglycemia and hypoglycemia.
The New England Journal of Medicine article, Outpatient Gatifloxacin Therapy and Dysglycemia in Older Adults, noted that:
“Between April 2002 and March 2004, we identified 788 patients treated for hypoglycemia within 30 days after antibiotic therapy. As compared with macrolide antibiotics, gatifloxacin was associated with an increased risk of hypoglycemia (adjusted odds ratio, 4.3; 95 percent confidence interval, 2.9 to 6.3). Levofloxacin was also associated with a slightly increased risk (adjusted odds ratio, 1.5; 95 percent confidence interval, 1.2 to 2.0), but no such risk was seen with moxifloxacin, ciprofloxacin, or cephalosporins. We then identified 470 patients treated for hyperglycemia within 30 days after antibiotic therapy. As compared with macrolides, gatifloxacin was associated with a considerably increased risk of hyperglycemia (adjusted odds ratio, 16.7; 95 percent confidence interval, 10.4 to 26.8), but no risk was noted with the other antibiotics. Risks were similar in the two studies regardless of the presence or absence of diabetes.”
A more recent study, that looked at a larger population than the NEJM study, Risk of Severe Dysglycemia Among Diabetic Patients Receiving Levofloxacin, Ciprofloxacin, or Moxifloxacin in Taiwan, found that all of the fluoroquinolones on the market increased the likelihood of both hyper and hypo glycemia in diabetic patients:
“A total of 78 433 diabetic patients receiving the antibiotics of interest were included in the study. The absolute risk of hyperglycemia per 1000 persons was 6.9 for moxifloxacin and 1.6 for macrolides. In contrast, the risk of hypoglycemia was 10.0 for moxifloxacin and 3.7 for macrolides. The adjusted odds ratios (AORs) and 95% confidence intervals (CIs) of levofloxacin, ciprofloxacin, and moxifloxacin compared with macrolides were 1.75 (1.12–2.73), 1.87 (1.20–2.93), and 2.48 (1.50–4.12), respectively, for hyperglycemia and 1.79 (1.33–2.42), 1.46 (1.07–2.00), and 2.13 (1.44–3.14), respectively, for hypoglycemia. Patients taking moxifloxacin faced a significantly higher risk of hypoglycemia than those receiving ciprofloxacin. A significant increase in the risk of hypoglycemia was also observed among patients receiving moxifloxacin concomitantly with insulin (AOR, 2.28; 95% CI, 1.22–4.24).”
As mentioned in the Temafloxacin section of this post, fluoroquinolone use has been linked to development of diabetes. Given that all fluoroquinolones cause blood-sugar dysregulation, and two fluoroquinolones have been removed from the market because they caused severe blood-sugar fluctuations, perhaps fluoroquinolones are behind the dramatic increase in both type 1 and type 2 diabetes over the last 30 years. It is a hypothesis that should certainly be looked into.
Conclusion
I struggle with whether or not I think all fluoroquinolones should be taken off the market. Even though I know that they are all dangerous, and sometimes even deadly, drugs, I also know that we are running out of antibiotics in our arsenal and that sometimes dangerous drugs are necessary in order to save a person’s life. I tend to think that Cipro/ciprofloxacin, Levaquin/levofloxacin, Avelox/moxifloxacin, Floxin/ofloxacin, and the other fluoroquinolones, should be severely restricted, and that there should be strict procedures followed when they are prescribed so that it is ensured that they will only be used in life-or-death situations where informed consent is given.
When looking at the fluoroquinolones that have been removed from the market, it always strikes me that they were removed from the market quickly after just a few deaths or a few studies that showed that they are dangerous drugs. The fluoroquinolones that remain on the market (Cipro/ciprofloxacin, Levaquin/levofloxacin, Avelox/moxifloxacin, Floxin/ofloxacin) have also killed people. According to an FDA review with the subject, “Pediatric Exclusivity Postmarketing Adverse Event Review,” between 12/20/1996 and 08/27/2008, 924 people were killed by Levaquin/levofloxacin, including three children. The figures for Cipro/ciprofloxacin, Avelox/moxifloxacin, and Floxin/ofloxacin are similar. So, why do Cipro/ciprofloxacin, Levaquin/levofloxacin, Avelox/moxifloxacin, Floxin/ofloxacin have such staying power? Why are they still on the market when Temafloxacin/Omniflox, Raxar/grepafloxacin, Zagam /Sparfloxacin, Trovan/Trovafloxacin, and Tequin/Gatifloxacin have been removed from the market? I don’t know the answers to those questions–I wish I did. It seems to me that the FDA used to be a stronger, more independent, more effective organization than it is today, and that it used to actually pull dangerous drugs from the market.
Rather than removing dangerous fluoroquinolones from the market, or even imposing meaningful restrictions on the fluoroquinolones that remain on the market, the FDA has instead chosen to increase the size of the fluoroquinolone warning labels. As I have noted before, changed warning labels open the door for lawsuits and that’s a good thing, but it is overall a useless move that is devoid of real change. Not enough doctors or patients read warning labels, and they are a lousy way to communicate the real risks of pharmaceuticals.
The fluoroquinolones that remain on the market are not significantly different from the fluoroquinolones that have been removed from the market. Updating warning labels isn’t keeping people from getting hurt by these dangerous drugs. I understand hesitation to remove them from the market completely, but there should be significant restrictions put on their use. Right now they are not being used prudently or appropriately. That must change. Too many people are being hurt by these dangerous drugs.










… [Trackback]
[…] Read More on on that Topic: floxiehope.com/fluoroquinolones-removed-from-the-market/ […]
… [Trackback]
[…] Here you can find 96357 more Information to that Topic: floxiehope.com/fluoroquinolones-removed-from-the-market/ […]
… [Trackback]
[…] Read More Info here to that Topic: floxiehope.com/fluoroquinolones-removed-from-the-market/ […]
… [Trackback]
[…] There you will find 82403 additional Information to that Topic: floxiehope.com/fluoroquinolones-removed-from-the-market/ […]
… [Trackback]
[…] Find More on to that Topic: floxiehope.com/fluoroquinolones-removed-from-the-market/ […]
… [Trackback]
[…] Info to that Topic: floxiehope.com/fluoroquinolones-removed-from-the-market/ […]
… [Trackback]
[…] Find More on to that Topic: floxiehope.com/fluoroquinolones-removed-from-the-market/ […]
… [Trackback]
[…] Find More Info here to that Topic: floxiehope.com/fluoroquinolones-removed-from-the-market/ […]
… [Trackback]
[…] Read More to that Topic: floxiehope.com/fluoroquinolones-removed-from-the-market/ […]
… [Trackback]
[…] Here you will find 49863 more Info on that Topic: floxiehope.com/fluoroquinolones-removed-from-the-market/ […]
… [Trackback]
[…] Find More Information here to that Topic: floxiehope.com/fluoroquinolones-removed-from-the-market/ […]
… [Trackback]
[…] Read More on to that Topic: floxiehope.com/fluoroquinolones-removed-from-the-market/ […]
… [Trackback]
[…] Find More on to that Topic: floxiehope.com/fluoroquinolones-removed-from-the-market/ […]