Following is a letter that I (Lisa Bloomquist) wrote to the European Medicines Agency (EMA) Committee for Medicinal Products for Human Use (CHMP). The CHMP will be reviewing fluoroquinolones starting on November 12, 2018, and they will make recommendations for use, marketing, and restriction of fluoroquinolones. Please consider sending a similar letter to them before 11/12/18. Contact information for all CHMP members can be found HERE.
Dear CHMP Reviewers,
Thank you for thoughtfully reviewing fluoroquinolones and for considering the following information.
Fluoroquinolone antibiotics are causally associated with tendon ruptures, serious psychiatric disturbances, blood-sugar irregularities, peripheral neuropathy, autonomic nervous system dysfunction, disabling multi-symptom chronic illness, and many other symptoms that are both listed on the US FDA warning labels and noted in the many patient reports that can be found in published case-reports, testimonials provided by victims, and anecdotes. The devastating and disabling effects of fluoroquinolone antibiotics were brought to the attention of the EMA during the PRAC hearing on the 13th of June 2018. It is my hope that you have listened to the patient testimonials presented to the PRAC, and that you are familiar with the severity of fluoroquinolone toxicity symptoms. In this letter, I will present some mechanisms through which fluoroquinolones lead to the symptoms noted above. I hope that you take these mechanisms into consideration when reviewing fluoroquinolones and making a judgement about their marketing and availability.
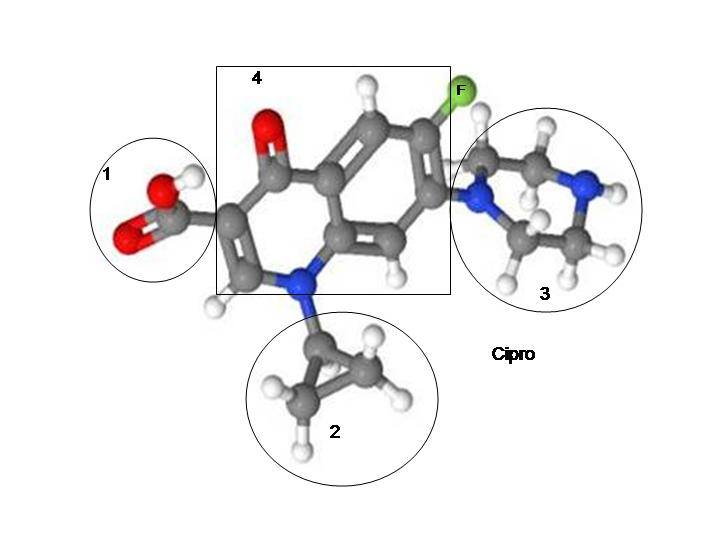
Fluoroquinolone Damage Mechanism 1 – Topoisomerase Interruption
The US FDA warning label for ciprofloxacin notes that, “The bactericidal action of ciprofloxacin results from inhibition of the enzymes topoisomerase II (DNA gyrase) and topoisomerase IV (both Type II topoisomerases), which are required for bacterial DNA replication, transcription, repair, and recombination.”
Fluoroquinolones are topoisomerase interrupters, and thus, as intended, they disrupt the process of bacterial DNA and RNA replication.
Though it is claimed that fluoroquinolones disrupt bacterial DNA not human nuclear DNA, this argument does not take into consideration the importance of bacterial DNA in human health, the fact that mitochondrial DNA is similar in structure to bacterial DNA, or the potential for promiscuous binding of fluoroquinolones to human nuclear DNA.
Fluoroquinolone Damage Mechanism 2 – Depletion of Mitochondrial DNA
Several studies have noted that fluoroquinolone antibiotics deplete mitochondrial DNA. In “Ciprofloxacin impairs mitochondrial DNA replication initiation through inhibition of Topoisomerase 2” (1) it is noted that:
“Loss of Top2β or its inhibition by ciprofloxacin results in accumulation of positively supercoiled mtDNA, followed by cessation of mitochondrial transcription and replication initiation, causing depletion of mtDNA copy number. These mitochondrial effects block both cell proliferation and differentiation, possibly explaining some of the side effects associated with fluoroquinolone antibiotics.”
Similar findings were published in 1996 in the article, “Delayed cytotoxicity and cleavage of mitochondrial DNA in ciprofloxacin-treated mammalian cells” (2).
Fluoroquinolone Damage Mechanism 3 – Increase in ROS and depletion of antioxidants
The study, “Oxidative Stress Induced by Fluoroquinolones on Treatment for Complicated Urinary Tract Infections in Indian Patients” (3) notes that fluoroquinolones decrease superoxide dismutates (SODs) and glutathione, and increase lipid peroxide levels.
Fluoroquinolone Damage Mechanism 4 – Neurotransmitter disruption and GABA inhibition
Fluoroquinolones are known to inhibit the activity of the neurotransmitter GABA, and to disrupt other neurotransmitter activities. The article, “Ciprofloxacin-induced neurotoxicity: evaluation of possible underlying mechanisms” (4) notes the following in its abstract:
Ciprofloxacin (CPX) is a fluoroquinolone antibiotic used for treating respiratory, urinary tract, gastrointestinal and abdominal infections. There are only a limited number of studies related to neurological adverse effects of this drug in therapeutic doses. Therefore, in the present study, we aimed to investigate the influence of CPX, when administered at pharmacological doses, on behavioral parameters of rats and the probable underlying mechanisms. CPX was administered in single oral daily doses of 20 and 50 mg/kg for 14 days in rats. CPX-induced depression and anxiety were evaluated by modified forced swimming test and elevated plus maze test, respectively. Also, spontaneous locomotor activity and motor coordination were assessed by activity cage and Rota-rod apparatus. Effects of CPX administration on brain serotonin, dopamine, γ-amino-butyric acid (GABA), glutamate, adrenaline and noradrenaline levels were determined by high performance liquid chromatography (HPLC) analysis. Contribution of oxidative stress to the changes induced by CPX administration was evaluated by measuring brain catalase, superoxide dismutase, glutathione (GSH) and malondialdehyde (MDA) levels. Our results indicated that depression-like and anxiety-like behaviors were observed only in the 50 mg/kg CPX-administered group with simultaneous decreases in the brain serotonin and GABA levels. In addition, in the brain homogenates of CPX-administered groups, increased MDA as well as decreased GSH and catalase activity with respect to their controls, indicated enhanced oxidative stress and weakened antioxidant defense system. In conclusion, repeated pharmacological doses of CPX were found to induce neurological toxicity. Also, altered brain neurotransmitter levels and increased oxidative stress observed in our study were thought to be the possible underlying mechanisms of ciprofloxacin-induced neurotoxicity.
Several studies, including “Benzodiazepine tolerance, dependency, and withdrawal syndromes and interactions with fluoroquinolone antimicrobials” (5) have noted that fluoroquinolone toxicity symptoms mimic those of benzodiazepine withdrawal.
Fluoroquinolone Damage Mechanism 5 – Depletion of Magnesium and Iron
The article, “Integrins on joint cartilage chondrocytes and alterations by ofloxacin or magnesium deficiency in immature rats” (6) notes that, “Recently, we showed that magnesium deficiency induces lesions in knee joint cartilage from 5-week-old rats that are very similar to ofloxacin-induced cartilage defects. We concluded that quinolone-induced arthropathy is probably due to chelation of magnesium and thus a deficit in functionally available magnesium in joint cartilage (Stahlmann et al. 1995).”
The article, “Nonantibiotic Effects of Fluoroquinolones in Mammalian Cells” (7) notes that, “Here, we show that the FQ drugs norfloxacin, ciprofloxacin, and enrofloxacin are powerful iron chelators comparable with deferoxamine, a clinically useful iron-chelating agent.”
Both cellular magnesium and iron are necessary for multiple enzymatic reactions, and they are necessary for health. Fluoroquinolones deplete both magnesium and iron, and may deplete other crucial minerals too.
Fluoroquinolone Damage Mechanism 6 – Microbiome Destruction
The importance of the gut microbiome has recently been uncovered. As a powerful class of antibiotics, fluoroquinolones disrupt the balance of gut microbiota in many ways. The consequences of gut microbiome disruption are now being uncovered. A disrupted gut microbiome has been linked to various diseases from Parkinson’s to Autism.
Fluoroquinolone Damage Mechanism 7 – Fluorine
Fluoroquinolones are fluorinated drugs, and it is known that fluorine displaces iodine, an element that is essential in the synthesis of thyroid hormones. Excess fluorine is linked to skeletal fluorosis (8), lowered IQ (9), and other health maladies. A significant amount of information about the harm that fluoride does can be found on the Fluoride Action Network web site, www.fluoridealert.org.
Additionally, it is recommended that the question of whether fluoroquinolones are metabolized into fluoroacetate be explored further.
Fluoroquinolone Damage Mechanism 8 – Thyroid Hormone Disruption
A significant amount of information about the connections between fluoroquinolones and thyroid hormone disruption can be found on the web site www.fluoroquinolonethyroid.com, and a summary of the connections can be found onhttp://www.hormonesmatter.com/fluoroquinolone-antibiotics-thyroid-problems-connection/.
Thyroid hormone disruption can lead to multi-symptom chronic illness, and most people suffering from fluoroquinolone toxicity would classify their illness as both multi-symptom and chronic. The connections between fluoroquinolone antibiotics and thyroid hormone disruption should be explored further.
Fluoroquinolone Damage Mechanism 9 – Epigenetic Changes
The article, “Epigenetic side-effects of common pharmaceuticals: A potential new field in medicine and pharmacology” (10) notes that:
“Interestingly, extensive changes in gene expression were found in articular cartilage of rats receiving the quinolone antibacterial agent ofloxacin, suggesting a potential epigenetic mechanism for the arthropathy caused by these agents. It has also been documented that the incidence of hepatic and dysrhythmic cardiovascular events following use of fluoroquinolones is increased compared to controls, suggesting the possibility of persistent gene expression changes in the liver and heart.”
Additionally, the published letter, “Hereditary Neuropathy Unmasked by Levofloxacin” (11) notes that a course of levofloxacin triggered Charcot-Marie-Tooth disease in a patient. Charcot-Marie-Tooth disease is thought to be a purely genetic disease, but the possibility exists that fluoroquinolone antibiotics are unmasking the disease.
Fluoroquinolone Damage Mechanism 10 – Increased MMP Expression
The article, “Ciprofloxacin enhances the stimulation of matrix metalloproteinase 3 expression by interleukin‐1β in human tendon‐derived cells” (12) notes that, “Ciprofloxacin enhances the stimulation of matrix metalloproteinase 3 expression by interleukin‐1β in human tendon‐derived cells.” This increase in MMP expression may have deleterious effects on all collagen and connective tissues.
Other potential damage mechanisms for fluoroquinolones include triggering mast cell activation, post-hepatic syndrome and liver damage, oxalate overload, extreme sensitivity to quinolones in the environment, calcium and/or potassium channel shifts, and many other possibilities. (http://fluoroquinolonethyroid.com/book_page/additional-mechanisms-to-consider/)
Exactly why some people experience devastating adverse reactions to fluoroquinolones is unknown. However, it is known and well-documented that fluoroquinolones cause a myriad of serious and severe adverse effects. I ask you to please thoughtfully consider each of the above mechanisms for fluoroquinolone damage when evaluating fluoroquinolones.
Thank you for your thought and consideration.
Sincerely,
Lisa Bloomquist
Durango, Colorado
USA
References:
- Anu Hangas, Koit Aasumets, Nina J Kekäläinen, Mika Paloheinä, Jaakko L Pohjoismäki, Joachim M Gerhold, Steffi Goffart; Ciprofloxacin impairs mitochondrial DNA replication initiation through inhibition of Topoisomerase 2, Nucleic Acids Research, Volume 46, Issue 18, 12 October 2018, Pages 9625–9636, https://doi.org/10.1093/nar/gky793
- Delayed cytotoxicity and cleavage of mitochondrial DNA in ciprofloxacin-treated mammalian cells. J W Lawrence, D C Claire, V Weissig and T C Rowe. Molecular Pharmacology November 1, 1996, 50 (5) 1178-1188.
- Oxidative Stress Induced by Fluoroquinolones on Treatment for Complicated Urinary Tract Infections in Indian Patients. V Talla and PR Veerareddy. J Young Pharm. 2011 Oct-Dec; 3(4): 304–309. doi: [10.4103/0975-1483.90242: 10.4103/0975-1483.90242]
- Sinem Ilgin, Ozgur Devrim Can, Ozlem Atli, Umut Irfan Ucel, Erol Sener & Ilkay Guven (2015) Ciprofloxacin-induced neurotoxicity: evaluation of possible underlying mechanisms, Toxicology Mechanisms and Methods, 25:5, 374-381, DOI: 10.3109/15376516.2015.1026008
- Benzodiazepine tolerance, dependency, and withdrawal syndromes and interactions with fluoroquinolone antimicrobials. Br J Gen Pract. 2008;58(550):365-6.
- Integrins on joint cartilage chondrocytes and alterations by ofloxacin or magnesium deficiency in immature rats. Förster, C., Kociok, K., Shakibaei, M. et al. Arch Toxicol (1996) 70: 261. https://doi.org/10.1007/s002040050272
- Badal S, Her YF, Maher LJ. Nonantibiotic Effects of Fluoroquinolones in Mammalian Cells. J Biol Chem. 2015;290(36):22287-97.
- Skeletal fluorosis in relation to drinking water in rural areas of West Azerbaijan, Iran Ali Akbar Mohammadi, Mahmood Yousefi, Mehdi Yaseri, Mohsen Jalilzadeh & Amir Hossein Mahvi Scientific Reports volume 7, Article number: 17300 (2017)
- Prenatal Fluoride Exposure and Cognitive Outcomes in Children at 4 and 6–12 Years of Age in Mexico. Morteza Bashash et al. Published:19 September 2017CID: 097017https://doi.org/10.1289/EHP655
- Epigenetic side-effects of common pharmaceuticals: A potential new field in medicine and pharmacology. Antonei B. Csoka and Moshe Szyf. Medical Hypotheses Volume 73, Issue 5, November 2009, Pages 770-780.https://doi.org/10.1016/j.mehy.2008.10.039
- Panas, M., Karadima, G., Kalfakis, N., & Vassilopoulos, D. (2011). Hereditary Neuropathy Unmasked by Levofloxacin. Annals of Pharmacotherapy, 45(10), 1312–1313. https://doi.org/10.1345/aph.1P786
- Ciprofloxacin enhances the stimulation of matrix metalloproteinase 3 expression by interleukin‐1β in human tendon‐derived cells. Anthony N. Corps et al. Arthritis and Rheumatology. Volume46, Issue11. November 2002 Pages 3034-3040. https://doi.org/10.1002/art.10617









… [Trackback]
[…] Find More here to that Topic: floxiehope.com/letter-to-the-ema/ […]
… [Trackback]
[…] Read More to that Topic: floxiehope.com/letter-to-the-ema/ […]
… [Trackback]
[…] Info to that Topic: floxiehope.com/letter-to-the-ema/ […]
… [Trackback]
[…] Read More to that Topic: floxiehope.com/letter-to-the-ema/ […]
… [Trackback]
[…] Information on that Topic: floxiehope.com/letter-to-the-ema/ […]
… [Trackback]
[…] Here you can find 23823 more Info on that Topic: floxiehope.com/letter-to-the-ema/ […]
… [Trackback]
[…] Info on that Topic: floxiehope.com/letter-to-the-ema/ […]
… [Trackback]
[…] There you can find 22824 more Info on that Topic: floxiehope.com/letter-to-the-ema/ […]
… [Trackback]
[…] Information to that Topic: floxiehope.com/letter-to-the-ema/ […]
… [Trackback]
[…] Here you can find 21352 additional Information to that Topic: floxiehope.com/letter-to-the-ema/ […]
… [Trackback]
[…] Read More on to that Topic: floxiehope.com/letter-to-the-ema/ […]
… [Trackback]
[…] Read More Information here to that Topic: floxiehope.com/letter-to-the-ema/ […]
… [Trackback]
[…] Info on that Topic: floxiehope.com/letter-to-the-ema/ […]
… [Trackback]
[…] Info to that Topic: floxiehope.com/letter-to-the-ema/ […]
… [Trackback]
[…] Here you can find 56383 additional Information on that Topic: floxiehope.com/letter-to-the-ema/ […]
… [Trackback]
[…] Here you will find 21755 additional Information on that Topic: floxiehope.com/letter-to-the-ema/ […]