
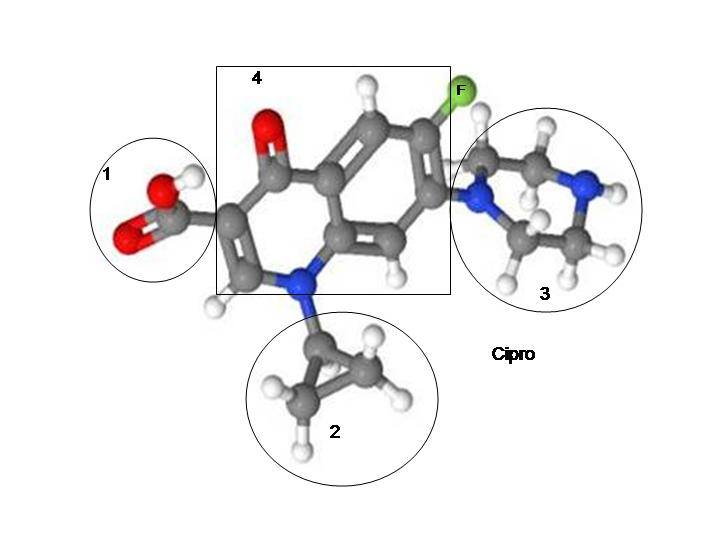
An excellent article about the effects of ciprofloxacin (a fluoroquinolone antibiotic) on mitochondrial DNA was recently published in the journal, Nucleic Acids Research. The article, Ciprofloxacin impairs mitochondrial DNA replication initiation through inhibition of Topoisomerase 2, by Anu Hangas, Koit Aasumets, Nina J Kekäläinen, Mika Paloheinä, Jaakko L Pohjoismäki, Joachim M Gerhold, and Steffi Goffart, gives a great amount of insight into the damage that ciprofloxacin does to mitochondria, and I recommend that you read it (linked through the article title). I’m going to go over the article in this post, and point out some of the more interesting findings.
First, a bit of background information to help readers to understand the article.
Mitochondria are the energy centers of our cells. There are over ten million billion mitochondria in the human body (Lane p. 1). Each cell (with a few exceptions) contains an average of 300-400 mitochondria that are responsible for generating cellular energy through a process called ATP (Adenosine Triphosphate). Mitochondria regulate energy production, aging, epigenetic signaling between and within cells and many other important functions. Proper functioning of mitochondria is vital, and when mitochondria are not operating properly, a wide range of disease states can ensue (2).
Mitochondria have their own DNA (mtDNA) that is separate from (though it interacts with) nuclear DNA. The structure of mtDNA is similar to that of bacterial DNA, and it is widely thought that mitochondria descended from ancient bacteria. The similarities between bacteria and mitochondria should make everyone take pause to think about how antibiotics of all kinds are affecting mitochondrial health. This post, and the article that it is based on, only focuses on the effects of ciprofloxacin, a fluoroquinolone antibiotic, on mitochondrial health, but if you want to read about the effects of other antibiotics on mitochondria, the article “Bactericidal Antibiotics Induce Mitochondrial Dysfunction and Oxidative Damage in Mammalian Cells” is a great place to start.
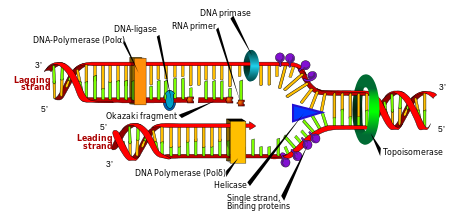
There are enzymes in our cells called topoisomerases. According to the wikipedia article for topoisomerase:
Topoisomerases are enzymes that participate in the overwinding or underwinding of DNA. The winding problem of DNA arises due to the intertwined nature of its double-helical structure. During DNA replication and transcription, DNA becomes overwound ahead of a replication fork. If left unabated, this torsion would eventually stop the ability of DNA or RNA polymerases involved in these processes to continue down the DNA strand.
In order to prevent and correct these types of topological problems caused by the double helix, topoisomerases bind to DNA and cut the phosphate backbone of either one or both the DNA strands. This intermediate break allows the DNA to be untangled or unwound, and, at the end of these processes, the DNA backbone is resealed again. Since the overall chemical composition and connectivity of the DNA do not change, the DNA substrate and product are chemical isomers, differing only in their global topology, resulting in the name for these enzymes. Topoisomerases are isomerase enzymes that act on the topology of DNA.[1]
Bacterial topoisomerases and human topoisomerases proceed via similar mechanisms for managing DNA supercoils.
The mechanism of action for all fuoroquinolones is that they are topoisomerase interruptors. The FDA warning label for ciprofloxacin states that the mechanism of action for ciprofloxacin is, “The bactericidal action of ciprofloxacin results from inhibition of the enzymes topoisomerase II (DNA gyrase) and topoisomerase IV (both Type II topoisomerases), which are required for bacterial DNA replication, transcription, repair, and recombination.”
Here is a video that describes how fluoroquinolones work, and how they interrupt topoisomerase and thus interrupt the process of bacterial (and mitochondrial, as we shall discuss below) DNA replication.
I have argued, and I believe, that EVERY drug that is a topoisomerase interruptor, should be thought of as a chemotherapy drug. All other topoisomerase interrupting drugs ARE chemo drugs. But fluoroquinolones are thought of as antibiotics, and handed out as if they are inconsequential. They are extremely consequential though, and they are hurting too many people. More information on fluoroquinolones being chemo drugs can be found in the post, “Cipro, Levaquin and Avelox are Chemo Drugs.”
Now to highlight some of the important parts of Ciprofloxacin impairs mitochondrial DNA replication initiation through inhibition of Topoisomerase 2.
The abstract of the article, Ciprofloxacin impairs mitochondrial DNA replication initiation through inhibition of Topoisomerase 2, notes that:
“Loss of Top2β or its inhibition by ciprofloxacin results in accumulation of positively supercoiled mtDNA, followed by cessation of mitochondrial transcription and replication initiation, causing depletion of mtDNA copy number. These mitochondrial effects block both cell proliferation and differentiation, possibly explaining some of the side effects associated with fluoroquinolone antibiotics.”
When you look into the multiple roles of mitochondria–from controlling cellular energy production to aging, and the links between mitochondrial damage and various multi-symptom chronic illnesses (from ME/CFS to autism to autoimmune diseases), yes, most definitely, the damaging effects of fluoroquinolones on mitochondria can certainly explain many, if not all, of the side effects associated with fluoroquinolone antibiotics.
The study found that, “In agreement with the in vitro assay, also HeLa cells treated with ciprofloxacin or doxorubicin rapidly accumulated supercoiled mtDNA (Figure 3A).”
This accumulation of supercoiled mtDNA led to a “change in topology” of the mitochondria, and a depletion of the mitochondrial DNA. Per the article:
“The change in topology caused by the inhibition of mitochondrial Top2 was connected with an impairment of mtDNA replication. 7S DNA, the 650bp ssDNA strand incorporated at the D-loop region of mtDNA, was rapidly depleted upon ciprofloxacin, ethidium bromide and doxorubicin treatment.”
Ciprofloxacin treatment not only depleted mtDNA, it also inhibited mtDNA synthesis:
“ciprofloxacin treatment reduced mtDNA copy number by 18% within 3 days (Figure 3C). As at the same time the growth rate of ciprofloxacin-treated cells was strongly reduced doubling time 170.2 h versus 22.7 h in untreated controls (Supplementary Figure S4), the observed depletion reflects a nearly complete inhibition of mtDNA synthesis.”
Ciprofloxacin treatment, and the resulting supercoiled mtDNA, also stalled mtDNA replication.
“Ciprofloxacin caused a strong reduction in these intermediates already after 2 h treatment (Figure 3E). After 20 h, this effect was clearly enhanced, with the strand-asynchronous intermediates being replaced by strand-coupled replication intermediates, a hallmark of mtDNA replication stalling (25,31–33).”
It was also found that ciprofloxacin inhibited the increase of mtDNA that typically comes with building muscle. It was found that:
“The impairment of mtDNA maintenance by ciprofloxacin not only disturbed cellular proliferation and the physiological increase of mtDNA copy number during muscle maturation, it also effectively impaired the fusion of confluent myoblasts to multinuclear myotubes (Figure 4E) and cell differentiation as indicated by the reduced expression of the heavy chain of Myosin II, a marker of differentiated skeletal muscle (Figure 4F).”
In the paragraph that the above quote was taken from, it was stated that “This increase (of mtDNA when muscle matures) was completely abolished by ciprofloxacin.” I’ve said it multiple times before, but, again, fluoroquinolones should NEVER be given to athletes (or anyone who values their ability to move, or have their heart beat).
In the article’s discussion section, this summary of the demonstrated damage done by ciprofloxacin was given:
“Ciprofloxacin caused a dramatic effect on mtDNA topology, blocking replication initiation, reducing copy number and inhibiting mitochondrial transcription (Figures 2B, 3A–E and 4A). Ciprofloxacin, the third most commonly used antibacterial antibiotic, stops the cleavage/re-ligation reaction of type II topoisomerases midway, generating double-strand breaks, persistent protein–DNA adducts and reduces also the overall enzyme activity (30). Its toxicity to mitochondria has been reported in various studies, suggesting a broad range of mechanisms including topoisomerase inhibition, oxidative stress, altered calcium handling and photosensitization (38–40). In our study, we observed ciprofloxacin to clearly reduce Top2 topoisomerase activity both in vitro and in vivo, but did not find any indication of increased mtDNA double-strand breaks (Figure 3A–C). However, ciprofloxacin did impair the overall mtDNA integrity in post-mitotic cells (Figure 4D). As our detection method (long-range PCR) does not distinguish between strand-breaks, abasic sites or base alterations inhibiting Taq polymerase, the observed effect might be caused by oxidative damage, which fluoroquinolones have been reported to induce in a variety of cell types (41,42).”
And the study’s authors also surmise that many of the severe adverse effects of fluoroquinolones are due to the depletion of mtDNA caused by the drugs:
“The severe side effects of ciprofloxacin and other fluoroquinolones include tendinopathies such as tendon rupture, joint inflammation, muscle weakness, central and peripheral neuropathies, epilepsy and psychological symptoms such as depression. These symptoms have been proposed to be connected to enhanced oxidative stress (42,54,55), but the molecular mechanism remained unclear. The reduction of mtDNA copy number and mitochondrial transcription caused by the altered topology of mtDNA might result in severe dysregulation of the electron transport chain complexes, as known to occur under ciprofloxacin treatment (56), lead to respiratory chain dysfunction and cause the observed enhanced oxidative stress.
Ciprofloxacin has also been reported to interfere with physiologically significant cell differentiation processes, such as spermatogenesis (57), brain development (41), bone mineralization (58), as well as to induce renal toxicity and heart arrhythmia (59). While the molecular mechanisms of these adverse effects are yet unclear, mitochondria play a central role in all of these physiological processes, making mitochondrial impairment a likely culprit for the disturbed cellular physiology.”
Throughout the article, the effects of ciprofloxacin are compared to the effects of another topoisomerase interrupting drug, doxorubicin. Per its wikipedia post, Doxorubicin “is a chemotherapy medication used to treat cancer.[3] This includes breast cancer, bladder cancer, Kaposi’s sarcoma, lymphoma, and acute lymphocytic leukemia.” The authors of Ciprofloxacin impairs mitochondrial DNA replication initiation through inhibition of Topoisomerase 2 noted that, “Interestingly, doxorubicin had a similar, but milder inhibitory effect on mtDNA replication than ciprofloxacin.” Why, yes, it is interesting that a drug that is marketed and dispensed as an antibiotic is more damaging than a similar drug that is marketed and dispensed as a chemotherapy drug. It’s very interesting indeed. It is also interesting that another topoisomerase interrupting chemotherapeutic drug, topotecan, was found to increase the expression of genes related to autism (“Topoisomerases facilitate transcription of long genes linked to autism“).
The Ciprofloxacin impairs mitochondrial DNA replication initiation through inhibition of Topoisomerase 2, authors conclude their article with two points. First, that very little is known about the consequences of mtDNA supercoiling. “Although central in bacterial genome maintenance, the whole phenomena of DNA supercoiling and its functional implications are virtually unstudied in mitochondria and calls for future research.” Yes, future research is needed, and better late than never. But nalidixic acid, the backbone of all fluoroquinolone antibiotics, was first used clinically in 1967. Shame on the medical and scientific communities for not studying the effects of fluoroquinolones on mtDNA earlier. We should have known more about the consequences of these drugs long before millions of prescriptions had been doled out, and millions of people affected.
Second, the authors of Ciprofloxacin impairs mitochondrial DNA replication initiation through inhibition of Topoisomerase 2 conclude by stating, “As fluoroquinolone antibiotics are widely used and effective drugs against a number of important bacterial pathogens, their dosage, systemic enrichment and side-effects should be reviewed in the mitochondrial context, and their clinical use should be considered with great care.” Yes, indeed, the effects of fluoroquinolones on mitochondria should be given long, hard, thoughtful consideration by every doctor, pharmacist, scientist, and every relevant person in the FDA and other regulatory agencies.
Ciprofloxacin impairs mitochondrial DNA replication initiation through inhibition of Topoisomerase 2 is an eye-opening article with groundbreaking research. Yes, more research needs to be done. But the research that has been done, that is described in the article, is greatly appreciated. Thank you to all the authors – Anu Hangas, Koit Aasumets, Nina J Kekäläinen, Mika Paloheinä, Jaakko L Pohjoismäki, Joachim M Gerhold, and Steffi Goffart.









… [Trackback]
[…] Read More Information here to that Topic: floxiehope.com/new-study-finds-that-ciprofloxacin-depletes-mitochondrial-dna/ […]
… [Trackback]
[…] Read More Info here on that Topic: floxiehope.com/new-study-finds-that-ciprofloxacin-depletes-mitochondrial-dna/ […]
… [Trackback]
[…] Read More on that Topic: floxiehope.com/new-study-finds-that-ciprofloxacin-depletes-mitochondrial-dna/ […]
… [Trackback]
[…] Here you will find 24499 more Info to that Topic: floxiehope.com/new-study-finds-that-ciprofloxacin-depletes-mitochondrial-dna/ […]
… [Trackback]
[…] Read More Information here on that Topic: floxiehope.com/new-study-finds-that-ciprofloxacin-depletes-mitochondrial-dna/ […]