What is the connection between fluoroquinolone toxicity and mast cell activation / histamine intolerance? Can fluoroquinolones trigger mast cell activation and histamine intolerance?
The symptoms of mast cell activation are similar to those of fluoroquinolone toxicity. According to Mastocytosis Society Canada, the symptoms of mast cell activation are:
skin lesions or sores, skin rash, spots, redness, hives, persistent fatigue, itching, flushing & severe sweating, joint, bone pain, headaches, tachycardia (racing heartrate), eyes tearing/dry, eye pain, persistent body/tissue pain, difficulty exercising, vertigo, episodes of low body temperature, unexplained Vitamin B12 deficiency, scents/odors/chemical reactions, difficult menses (females), numbness & tingling in face and extremities, skin feels on fire, unexplained anxiety, sudden drops in blood pressure, fainting, persistent diarrhea, vomiting, unexplained weight loss, cognitive impairment, sinus problems, chest pain, vision problems, hair loss, mouth sores, nausea, swelling & inflammation, odd reactions to insect stings, anesthesia difficulties, anemia, thyroid problems, decreased bone density, unexplained weakness, shortness of breath, sunlight sensitivity, temperature (hot/cold) sensitivity, difficulty with foods, drinks, anaphylactoid reactions, anaphylaxis, gastrointestinal pain, bloating, unexplained medication reactions, enlarged liver/spleen, liver/spleen/bladder/kidney pain, enlarged lymph nodes, frequent urination, recurring infections, neuropathic pain, constipation, iron deficiency, unexplained bruising, bleeding, malabsorption, intermittent tinnitus or hearing problems.
That’s a pretty comprehensive list of fluoroquinolone toxicity symptoms too. (Though, as I discussed with Dr. Wahls in episode 14 of The Floxie Hope Podcast, all of the multi-symptom, chronic diseases of modernity have more in common with each other than they don’t, and should probably all just be categorized as cellular dysfunction disorders and treated similarly.)
Several floxies who have been able to get a diagnosis from a doctor have come back with a diagnosis of mast cell activation, or a disease that is related to mast cells. For example, one floxie friend’s doctors have diagnosed him with eosinophilia, a disorder that is related to mast cells and histamine intolerance. Other floxies have been diagnosed as histamine intolerant, and instructed to go on a low-histamine diet. As noted above, many floxies have symptoms of mastocytosis, and it is possible that fluoroquinolones activate mast cells and trigger mastocytosis.
Mast cell disorders are considered to be rare, but, according to Mastocytosis Society Canada, “escalation in the prevalence of these patients worldwide has resulted in a flurry of medical research ongoing in numerous countries. This indicates that these disorders may not be rare, but rather have been commonly misidentified and unfortunately for patients worldwide, commonly undiagnosed. Since approximately 2005, every year there are new theories, classifications, and adjustments to the mastocytosis definitions due to escalation of patients presenting with these disorders worldwide.”
I found the following information connecting fluoroquinolones and mast cell activation / mastocytosis:
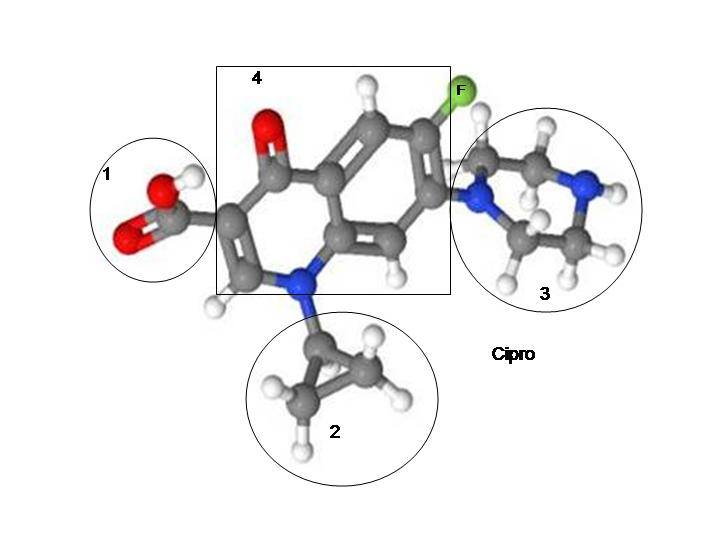
- From the International Journal of Tissue Reaction’s article, Effect of levofloxacin and ciprofloxacin injection on permeability of the tail vein in mice and skin microvasculature in rats, “These results suggest that LVFX and CPFX increase vascular permeability through the induction of histamine release from mast cells in rodents.” (LVFX is levofloxacin and CPFX is ciprofloxacin.)
- From the Journal of Pharmacy and Pharmacology’s article, Characterization of Histamine Release Induced by Fluoroquinolone Antibacterial Agents In-vivo and In-vitro, “Intravenous injection of levofloxacin and ciprofloxacin at 1–10 mg kg−1 produced dose-related elevations in plasma histamine level in anaesthetized dogs. In contrast, levofloxacin was devoid of plasma histamine increment in anaesthetized rats at 100 mg kg−1, whereas ciprofloxacin at the same dose caused endogenous histamine release. Levofloxacin and ciprofloxacin induced non-cytotoxic secretion of histamine from all mast cells tested in a concentration-dependent manner, whereas rat skin and peritoneal mast cells were thirty- to one-hundred-times less sensitive to the effect of fluoroquinolones as compared with the canine skin mast cells.” Note that in studies beagle puppies have been made lame by fluoroquinolones.
- From the Archives of Toxicology’s article, Differential response of mast cells separated from various organs and basophils of dogs to the fluoroquinolone antimicrobial levofloxacin, “Histamine releases induced by the fluoroquinolone antimicrobial levofloxacin (LVFX) were investigated using mast cells separated from various organs and peripheral basophils of dogs, being the most susceptible species to quinolone derivatives, in both in vivo and in vitro systems. An intravenous infusion of LVFX at 30 mg/kg over a 30-min period produced endogenous histamine release from 5 min, and a maximum at 30 min, in which the plasma LVFX concentration was approximately 50 µM. A close correlation (r=0.87, n=20) between histamine and LVFX concentrations in plasma during the infusion was observed. In the in vitro study, LVFX at 30 µM or more caused histamine release from mast cells separated from the liver and skin, but not from the gastric mucosa, lung, and peripheral basophils. More exactly, the liver mast cells were most susceptible to LVFX among the organs tested. On the other hand, compound 48/80, a prototype histamine liberator, elicited the histamine release from the liver or skin mast cells at 10 µg/ml, and the calcium ionophore A23187 at 1 µM exhibited the histamine release from the mast cells derived from all organs examined. Histochemical analysis revealed that the liver and skin mast cells had positive reaction for both alcian blue and safranin staining, but the gastric mucosa and lung mast cells were only positive for alcian blue staining, indicating that LVFX preferably activated the connective tissue-type mast cells rather than the mucosal-type mast cells. The degranulation of the liver and skin mast cells brought about by either LVFX or compound 48/80, unlike the calcium ionophore A23187, was blocked by pretreatment with pertussis toxin, suggesting the involvement of pertussis toxin-sensitive G proteins. The results obtained from the canine experiments strongly suggest that LVFX induces histamine release from the connective tissue-type mast cells distributed mainly in the liver, somewhat in the cutaneous tissue, through the activation of pertussis toxin-sensitive G proteins.”
The articles noted above are all from animal studies, not human studies, but they show that fluoroquinolones can activate mast cells and histamine release in mammals, and it’s reasonable to think that they may do the same things to humans that they do to dogs. Also, the similarity between fluoroquinolone toxicity symptoms and mastocytosis symptoms, though not a smoking gun, indicate that further studies of the affects of fluoroquinolones on mast cells should be done.
A few good resources for people with mastocytosis, and it’s possible that floxies are in that category, are:
- Dr. Theoharides web site
- Mastocytosis Society Canada web site
- The Low Histamine Chef web site
- Alison Vickery’s web site
I suspect that mast cells are profoundly affected by fluoroquinolones and that mast cell activation is a big part of fluoroquinolone toxicity. The potential options, and mechanisms for fluoroquinolone toxicity, are mind-boggling. Add mast cell activation to the list.








I hope drs begin to realize what these drugs can do to you. I’m 70 got floxed at age 65. Doe not know
What was happening to me. 3 different exposure to
Cipro. Did not Realize that was what was causing my skin reactions seizures trimmers anxiety weight loss sores mental dysfunction stiff joints etc.
Can this be reversed?
… [Trackback]
[…] Here you will find 83069 more Information on that Topic: floxiehope.com/can-fluoroquinolones-activate-mast-cells/ […]
… [Trackback]
[…] Find More Information here on that Topic: floxiehope.com/can-fluoroquinolones-activate-mast-cells/ […]
… [Trackback]
[…] Find More Info here to that Topic: floxiehope.com/can-fluoroquinolones-activate-mast-cells/ […]
… [Trackback]
[…] Find More Information here on that Topic: floxiehope.com/can-fluoroquinolones-activate-mast-cells/ […]
… [Trackback]
[…] Read More here on that Topic: floxiehope.com/can-fluoroquinolones-activate-mast-cells/ […]
… [Trackback]
[…] Read More to that Topic: floxiehope.com/can-fluoroquinolones-activate-mast-cells/ […]
… [Trackback]
[…] Read More on that Topic: floxiehope.com/can-fluoroquinolones-activate-mast-cells/ […]
… [Trackback]
[…] Info on that Topic: floxiehope.com/can-fluoroquinolones-activate-mast-cells/ […]
… [Trackback]
[…] Read More here on that Topic: floxiehope.com/can-fluoroquinolones-activate-mast-cells/ […]
… [Trackback]
[…] Read More here on that Topic: floxiehope.com/can-fluoroquinolones-activate-mast-cells/ […]
… [Trackback]
[…] Read More on that Topic: floxiehope.com/can-fluoroquinolones-activate-mast-cells/ […]
… [Trackback]
[…] Read More here to that Topic: floxiehope.com/can-fluoroquinolones-activate-mast-cells/ […]
… [Trackback]
[…] Here you will find 88210 more Info to that Topic: floxiehope.com/can-fluoroquinolones-activate-mast-cells/ […]
… [Trackback]
[…] Here you can find 70095 more Information to that Topic: floxiehope.com/can-fluoroquinolones-activate-mast-cells/ […]
… [Trackback]
[…] Read More Info here to that Topic: floxiehope.com/can-fluoroquinolones-activate-mast-cells/ […]