Overprescription of Antibiotics
I found this New York Times article, How to Stop Overprescribing Antibiotics, to be really interesting. Doctors know that antibiotic resistance is a serious problem–the word has gotten out sufficiently, but that knowledge hasn’t done much to change antibiotic prescribing patterns. Doctors are still overprescribing antibiotics, despite knowing that antibiotic resistance poses a significant threat to both modern medicine and human health.
I’m not sure what the root of this overprescribing is. It may be from a lack of knowledge of what ailments antibiotics should be prescribed for (many cases of prostatitis, as well as many sinus infections, aren’t bacterial), tradition (it’s the way it has “always” been done), a notion that antibiotics “can’t hurt,” patient pressure on the physician to do something, or if there’s another root to the problem.
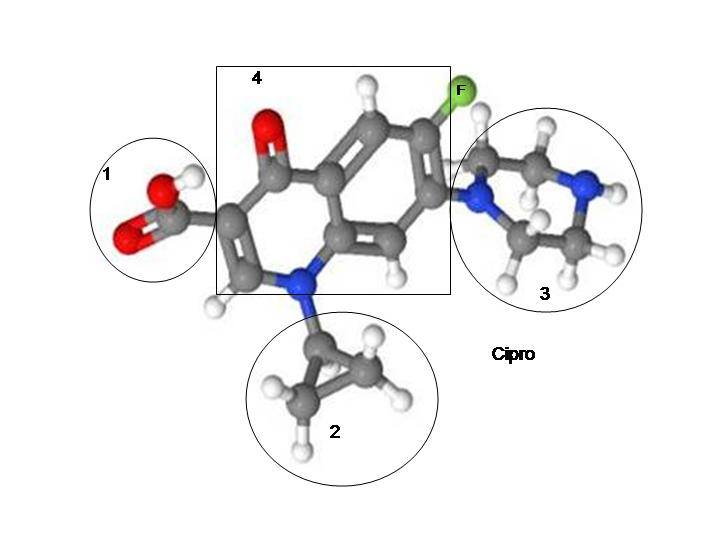
Antibiotic overprescription IS a problem though. It’s a problem not only because of bacterial resistance to antibiotics, but also because of the links between antibiotic use and many of the diseases of modernity, and because some popular antibiotics (FLUOROQUINOLONES in particular, but I’ve heard from people who have been devastated by other antibiotics too) are causing multi-symptom, chronic illnesses that are devastating people’s lives.
Overprescription of Fluoroquinolone Antibiotics
How can we get doctors to stop overprescribing fluoroquinolone antibiotics? The NYT article has some good insight and possible courses of action for floxie advocates.
“we asked a group of doctors to place a signed poster in their exam rooms pledging to follow standard guidelines on antibiotic prescription. This tactic, which pressured doctors to act consistently with their own publicly stated commitments, reduced inappropriate prescribing 20 percentage points relative to doctors in a control group who displayed a poster with generic information about antibiotic use.”
A 20% reduction in inappropriate prescribing is pretty good. At the very least, it’s a good place to start.
Guidelines for Prescribing Fluoroquinolones
What should the guidelines for fluoroquinolone (Cipro, Levaquin, Avelox, Floxin, and their generic equivalents) prescriptions be? My suggestions are:
- Only prescribe fluoroquinolones for verified infections.
- Only prescribe fluoroquinolones in life-or-death situations.
- Only prescribe fluoroquinolones if there is no safer antibiotic that can be tried.
- Review the warning label with the patient.
- Review the black box warning with the patient. Notify the patient that black box warnings are the most severe warning possible before a drug is removed from the market.
- Inform the patient that severe musculoskeletal problems have been experienced post-exposure to fluoroquinolones, including, but not limited to, tendon tears that occur months or years after exposure to the drug has stopped.
- Note that, per the FDA, “A review of the FDA Adverse Event Reporting System (FAERS) was performed to characterize a constellation of symptoms leading to disability that had been observed during FDA monitoring of fluoroquinolone safety reports. This constellation of symptoms will be referred to in this review as ‘fluoroquinolone-associated disability’ (FQAD). While most of the individual AEs that exist within FQAD are currently described in fluoroquinolone labeling, the particular constellation of symptoms across organ systems is not. Individuals with FQAD were defined as U.S. patients who were reported to be previously healthy and prescribed an oral fluoroquinolone antibacterial drug for the treatment of uncomplicated sinusitis, bronchitis, or urinary tract infection (UTI). To qualify, individuals had to have AEs reported in two or more of the following body systems: peripheral nervous system, neuropsychiatric, musculoskeletal, senses, cardiovascular and skin. These body systems were chosen as they had been observed to be frequently involved with the fluoroquinolone reports describing disability. In addition, the AEs had to have been reported to last 30 days or longer after stopping the fluoroquinolone, and had to have a reported outcome of disability.”
- Fluoroquinolones cause mitochondrial damage and dysfunction, and mitochondrial damage/dysfunction is linked to many diseases, including autoimmune diseases.
- Fluoroquinolone effects include serious psychiatric problems.
- Fluoroquinolones are a likely endocrine disruptor.
I suspect that if those guidelines were in every physician’s office, fluoroquinolone prescriptions would decrease significantly.
Present Alternatives to Antibiotics
The NYT article also notes:
“we showed that doctors tended to prescribe less aggressive medications when such options were presented more prominently (one by one, in a vertical column), with more aggressive options presented less prominently (grouped side by side, in a single category). Previous research suggested that listing alternatives individually made them appear more popular — and therefore more appropriate — than when they were grouped together. And indeed, we found that doctors were roughly 12 percent less likely to order more aggressive medications, such as antibiotics, if these options were grouped together, compared with when they were listed individually.”
I think that’s an excellent idea! Give the physician more information and the patient more options. Sounds great!
Use Social Pressure and Physician Psychology to Achieve Goals
Another approach mentioned in the NYT article is:
“In one approach, doctors received a monthly email informing them of their performance relative to that of their peers. Those with the lowest inappropriate antibiotic prescribing rates were congratulated for being ‘top performers.’ Doctors who were not top performers were told ‘You are not a top performer.’ The email also included a personalized count of unnecessary antibiotic prescriptions and the count for a typical top performer. This ‘peer comparison’ approach almost completely eliminated inappropriate prescribing: from 19.9 percent in the pre-intervention period to 3.7 percent during the post-intervention period — an 81 percent reduction.”
An 81% reduction is impressive and significant!
Peer comparison is powerful because it taps into doctor’s egos. For fluoroquinolones, I think that guilt should be tapped into as well, and with the low-ranking notification should be a story of someone suffering from fluoroquinolone toxicity. These stories may be anecdotal, but they are real stories of people being devastated by these drugs.
Public Accountability
Another approach to curbing antibiotic use mentioned is:
“whenever doctors prescribed an antibiotic that was not clearly called for by the diagnosis, the electronic health record system asked them to provide a short ‘antibiotic justification note.’ The note would be entered into the patient’s medical record and would be visible to others. Introducing this speed bump into the work flow, along with the prospect of social accountability, reduced the inappropriate prescribing rate from 23.2 percent to 5.2 percent — a 77 percent reduction.”
Public accountability is a good thing. This could work well for curbing unnecessary fluoroquinolone prescriptions.
Start Curbing Antibiotic Overprescription by Curbing Fluoroquinolone Overprescription
The article concludes that, “Taken together, our studies suggest that simple and inexpensive tactics, grounded in scientific insights about human behavior, can be extremely effective in addressing public health problems.”
I think that the methods noted above could effectively cut fluoroquinolone use too.
Maybe trying to curb overuse of all antibiotics is too much to take on. Perhaps taking on overuse of one category of antibiotics at a time is an effective thing to do. I suggest that those who are interested in curbing antibiotic overprescription start with fluoroquinolones.










… [Trackback]
[…] Find More Info here on that Topic: floxiehope.com/how-to-stop-overprescribing-fluoroquinolone-antibiotics/ […]
… [Trackback]
[…] Find More on to that Topic: floxiehope.com/how-to-stop-overprescribing-fluoroquinolone-antibiotics/ […]
… [Trackback]
[…] Here you will find 59283 more Info on that Topic: floxiehope.com/how-to-stop-overprescribing-fluoroquinolone-antibiotics/ […]
… [Trackback]
[…] Find More Info here on that Topic: floxiehope.com/how-to-stop-overprescribing-fluoroquinolone-antibiotics/ […]
… [Trackback]
[…] Information to that Topic: floxiehope.com/how-to-stop-overprescribing-fluoroquinolone-antibiotics/ […]
… [Trackback]
[…] Read More here on that Topic: floxiehope.com/how-to-stop-overprescribing-fluoroquinolone-antibiotics/ […]
… [Trackback]
[…] Find More to that Topic: floxiehope.com/how-to-stop-overprescribing-fluoroquinolone-antibiotics/ […]