This is a guest post written by Gary. You can read Gary’s story HERE. It contains a wonderful wealth of knowledge, insight, and advice.
Fluoroquinolone side effects are often multisymptom affecting a wide range of bodily functions, ie: CNS, Muscles, Tendons, Brain, etc (Halkin, 1988l Mattappalil and Mergenhagen, 2014; Menzies et al., 1999; Moorthy et al., 2008; Thomas and Reagan, 1996; etc)
The chronic, often multisymptom, effects are not well documented and are normally assigned (often multiple) different diagnosis by doctors, such as clinical depression, fibromyalgia, etc/ (Strauchman and Morningstar, 2012)
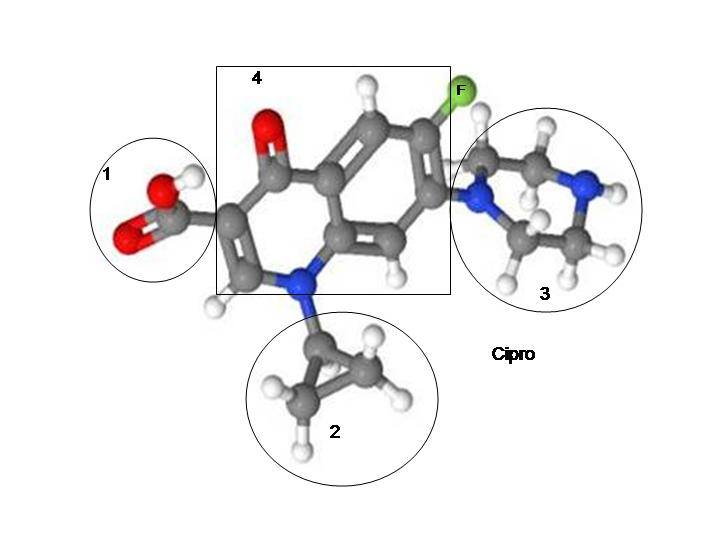
I argue the reason for the chronic effects is because the Fluoroquinolones are not metabolized correctly, or the are metabolized and the normal biological enzymes that are responsible for detoxification of xenobiotic substrates is impared. A xenobiotic is a synthetic chemical such as Levaquin, Cipro, pestacides, etc. It’s also likely that FQ exposure changes gene expressions relating to various cytochrome P-450s (which is responsible for metabolizing and detoxification) causing your body to accumulate toxic chemicals, being unable to remove them.
For example, According to Liang et al., (2015), Fish that were exposed to a specific FQ had changes to cytochrome P450 1A (CYP1A), cytochrome P-450 3A (CYP3A), glutathione S-transferase (GST), P-glycoprotein (P-gp), which are all responsible for metabolizing and/or removal of xenobiotics. Other animals exposed to FQs were shown to have changes in cytochrome P-450 sites – For example, Dogs exposed to FQs showed inhibiting only cytochrome P-450 3A (Regmi et al., 2005; 2007), Chickens (Shlosberg et al., 1997; Granfors et al., 2004). To be fair, this might not affect humans completely, but this would likely explain the delayed toxicity to the CNS and other parts of the body – Delayed toxicity for FQ patients are likely a result of impared detoxification pathways due to FQ exposure overall which means the body has a high level of xenobiotics that cannot be removed.
There are even a few case studies on /people/ to support this article. In a paper (Strauchman and Morningstar, 2012), a patient was prescribed Moxifloxacin in 2005 and developed a worsening set of symptoms (after inclusion of medication), such as episodic tachycardia, episodic dizziness, episodic shortness of breath, and chronically swollen glands. Additional symptoms included daily episodes of nausea, sweating, tremors, brain fog, blurred vision, panic attacks, and phonophobia. Over the course of 3 years, after Moxifloxacin treatment, her condition improved, modestly.
In 2011, the PCP diagnosed the patient with diverticulitis and prescribed her ciprofloxacin 500 mg – Over the course of the treatment, she started to experience all the previous symptoms from 2005 – including panic attacks, insomnia, blurred vision, tachycardia, and nausea. This episode additionally included diffuse musculoskeletal joint pain. The patient also reported that her elbows, wrists, and knees seemed to crack too easily and too often. (p.3). Full workup was ordered, including genetic testing which showed the following:
– Genetic polymorphism in the cytochrome P-450 pathway
– Genetic variations in the catechol-o-methyl transferase enzyme, the Nacetyl transferase enzyme, and the glutathione-s-transferase enzyme necessary for glutathione conjugation and phase II detoxification.
The patient was also tested for polychlorinated biphenyls and other volatile solvents. They found the patient to have elevated levels of ethylbenzene, xylene, and the pesticide dichlorodiphenyldichloroethylene. Although these levels could indicate environmental accumulation, impaired detoxification pathways may make this accumulation more of a contributing factor.
Fluoroquinolone treatment seems to affect enzymes possesses, causing reduced activity due to chelation of ions, such as Se2 [Selenium], Mg2 [Magnesium], Fe2/3+ [Iron] (Badal et al., 2015; Uivarosi, 2013; Seedher and Agarwal, 2010) which explains the chronic issues, as well as delayed toxicity (due in part to impaired detoxification)
Even more evidence that either FQs remain in the body, impairing detoxification of xenobiotics (or they contribute to impairment) is from a journal (Cohen, 2008) where a patient was on a 14 day course of Moxifloxacin and became disabled, for many years; His symptoms were Brain Fog, Cognitive Defects/memory loss, tingling and numbness in his legs, joint pains, Achilles pain, Chronic Fatigue, Weakness, to a degree that he could barely stand or walk; The patient began IV Based Antioxidant therapy, and his condition improved considerably (95%+ recovery within a month). It’s highly likely that the IV Antioxidant therapy activated/modulated cytochrome P-450 to allow the patients body to excrete the excessive, normal environmental xenobiotics (and including Moxifloxican) and the patient recovered.
Fluoroquinolones have a very high melting point, over 200C, which means the crystals they form are very stable in neutral pH. (Andriole et al., 2000). If FQs are stuck within the cells, then that means they are responsible with mitochondrial ETC leakage, causing depressed health effects (ie: Brain Fog from FQ exposure is likely caused by FQs interfering with ATP energy output, which affects the Brain’s homeostasis).
What causes the delayed toxicity? There are only 3 possible explanations.
– You have pre-existing genetic polymorphisms in cytochrome P450s (and others) that prevent you from metabolizing and/or excreting FQs – Which leads to various normal systems in the body to suffer for a long period of time. (FQ crystals are ‘stuck’ in your body)
– FQs /cause/ the polymorphisms because they chelate heavy metals that enzymes require for proper biological function, such as phase II detoxification. Once this happens, your body begins to accumulate xenobiotics and you develop delayed toxicity.
– FQs cause mitochrondia dysfunction with organs responsible for generting glutathione, causing your body to have extremely low levels of glutathione, leading to increased amounts of xenobiotics that you cannot remove.
If this behavior takes place, how do we prove it?
– Genetic testing is the only way to be sure you have these Genetic polymorphisms/Genetic Variations – Some sites out there do provide this.
– Liquid Chromatography-tandem mass spectrometry will need to be performed on blood samples from people currently damaged by FQs to see if any concentrations of it exist in plasma.
– Total GSH testing would likely show lower-than-expected glutathione levels in the body with someone that is disabled, because if FQs are embedded in the cells, they are likly decreasing ATP output of various organs.
How would we remove the FQs that are ‘stuck’ in the body?
– Ozone is able to remove FQs from water (Feng et al., 2016). Therefor, Ozone therapy might be an idea If this behavior of FQs takes place.
– Fluoroquinolones have a Michael acceptor in them, making them very electrophilic. The non-aromatic double bond could potentially be subject to nucleophilic attack via a Michael addition, so one removal strategy could be allowing ligating the fluoroquinolone/associated polymorphs to something that is readily transported across cell membranes and excreted. However, this would need to be drawn up on a computer simulation to see if this could be done, cost effectively.
– Prolonged IV Antioxidant therapy, as shown above, seems to reverse FQ toxicity in some patients but further testing will need to be done (A heavy metal toxscreen via blood to be tested for chemical insult will likely need to be ordered)
Pharmacogenomics is going to likely show who is compatible with FQs and who isn’t, down the road–once we identify specific SNP’s that are broken with us floxies, the /good/ news is, with CRISPR technology, those of us with pre-existing polymorphisms (pre/post-FQ) will likely be able to have them corrected with little to no side effects.
Data from the following:
Strauchman M, Morningstar MW. Fluoroquinolone toxicity symptoms in a patient presenting with low back pain. Clinics and Practice. 2012;2(4):e87. doi:10.4081/cp.2012.e87.
N. L. Regmi, A. M. Abd El-Aty, R. Kubota, S. S. Shah, and M. Shimoda, “Lack of inhibitory effects of several fluoroquinolones on cytochrome P-450 3A activities at clinical dosage in dogs,” Journal of Veterinary Pharmacology and Therapeutics, vol. 30, no. 1, pp. 37–42, 2007. · ·
N. L. Regmi, A. M. Abd El-Aty, M. Kuroha, M. Nakamura, and M. Shimoda, “Inhibitory effect of several fluoroquinolones on hepatic microsomal cytochrome P-450 1A activities in dogs,” Journal of Veterinary Pharmacology and Therapeutics, vol. 28, no. 6, pp. 553–557, 2005. · ·
M. D. Brand, R. L. Goncalves, A. L. Orr et al., “Suppressors of superoxide-H2O2 production at site IQ of mitochondrial complex I protect against stem cell hyperplasia and ischemia-reperfusion injury,” Cell Metabolism, vol. 24, no. 4, pp. 582–592, 2016. · ·
M. A. Simonin, P. Gegout-Pottie, A. Minn, P. Gillet, P. Netter, and B. Terlain, “Pefloxacin-induced Achilles tendon toxicity in rodents: biochemical changes in proteoglycan synthesis and oxidative damage to collagen,” Antimicrobial Agents and Chemotherapy, vol. 44, no. 4, pp. 867–872, 2000. · ·
Krzysztof Michalak, Aleksandra Sobolewska-Włodarczyk, Marcin Włodarczyk, Justyna Sobolewska, Piotr Woźniak, and Bogusław Sobolewski, “Treatment of the Fluoroquinolone-Associated Disability: The Pathobiochemical Implications,” Oxidative Medicine and Cellular Longevity, vol. 2017, Article ID 8023935, 15 pages, 2017. doi:10.1155/2017/8023935
J. M. Radandt, C. R. Marchbanks, and M. N. Dudley, “Interactions of fluoroquinolones with other drugs: mechanisms, variability, clinical significance, and management,” Clinical Infectious Diseases, vol. 14, no. 1, pp. 272–284, 1992.
H. H. M. Ma, F. C. K. Chiu, and R. C. Li, “Mechanistic investigation of the reduction in antimicrobial activity of ciprofloxacin by metal cations,” Pharmaceutical Research, vol. 14, no. 3, pp. 366–370, 1997.
N. Seedher and P. Agarwal, “Effect of metal ions on some pharmacologically relevant interactions involving fluoroquinolone antibiotics,” Drug Metabolism and Drug Interactions, vol. 25, no. 1–4, pp. 17–24, 2010.
H. Koga, “High-performance liquid chromatography measurement of antimicrobial concentrations in polymorphonuclear leukocytes,” Antimicrobial Agents and Chemotherapy, vol. 31, no. 12, pp. 1904–1908, 1987.
A. Pascual, I. García, S. Ballesta, and E. J. Perea, “Uptake and intracellular activity of trovafloxacin in human phagocytes and tissue-cultured epithelial cells,” Antimicrobial Agents and Chemotherapy, vol. 41, no. 2, pp. 274–277, 1997.
V. T. Andriole, The Quinolones – Third Edition, Acedemic Press, San Diego California, 2000.
S. Badal, Y. F. Her, and L. J. Maher 3rd, “Nonantibiotic effects of fluoroquinolones in mammalian cells,” The Journal of Biological Chemistry, vol. 290, no. 36, pp. 22287–22297, 2015.
J. Y. Lee, S. H. Lee, J. W. Chang, J. J. Song, H. H. Jung, and G. J. Im, “Protective effect of metformin on gentamicin-induced vestibulotoxicity in rat primary cell culture,” Clinical and Experimental Otorhinolaryngology, vol. 7, no. 4, pp. 286–294, 2014. · ·
Z. K. Salman, R. Refaat, E. Selima, A. El Sarha, and M. A. Ismail, “The combined effect of metformin and L-cysteine on inflammation, oxidative stress and insulin resistance in streptozotocin-induced type 2 diabetes in rats,” European Journal of Pharmacology, vol. 714, no. 1–3, pp. 448–455, 2013. · ·
A. I. Morales, D. Detaille, M. Prieto et al., “Metformin prevents experimental gentamicin-induced nephropathy by a mitochondria-dependent pathway,” Kidney International, vol. 77, no. 10, pp. 861–869, 2010. · ·
W. Chowanadisai, K. A. Bauerly, E. Tchaparian, A. Wong, G. A. Cortopassi, and R. B. Rucker, “Pyrroloquinoline quinone stimulates mitochondrial biogenesis through cAMP response element-binding protein phosphorylation and increased PGC-1alpha expression,” The Journal of Biological Chemistry, vol. 285, no. 1, pp. 142–152, 2010. · ·
T. Stites, D. Storms, K. Bauerly et al., “Pyrroloquinoline quinone modulates mitochondrial quantity and function in mice,” The Journal of Nutrition, vol. 136, no. 2, pp. 390–396, 2006.
Y. Huang, N. Chen, and D. Miao, “Biological effects of pyrroloquinoline quinone on liver damage in Bmi-1 knockout mice,” Experimental and Therapeutic Medicine, vol. 10, no. 2, pp. 451–458, 2015. · ·
M. Feng, L. Yan, X. Zhang et al., “Fast removal of the antibiotic flumequine from aqueous solution by ozonation: influencing factors, reaction pathways, and toxicity evaluation,” Science of The Total Environment, vol. 541, pp. 167–175, 2016
**












… [Trackback]
[…] Here you will find 45903 more Info on that Topic: floxiehope.com/persistent-fluoroquinolones-in-the-body-and-delayed-adverse-reactions/ […]