I’m not a doctor. If you want to know exactly what medications you should or shouldn’t take given your personal medical history, please ask your doctor. Please also know that these are not hard and fast rules for every floxie. Given that there is so little research into fluoroquinolone toxicity, there aren’t many definitive rules for what pharmaceuticals people can and cannot take post-flox. Following is information though, and with information, perhaps you can make a more informed choice about which drugs to take and which ones to avoid.
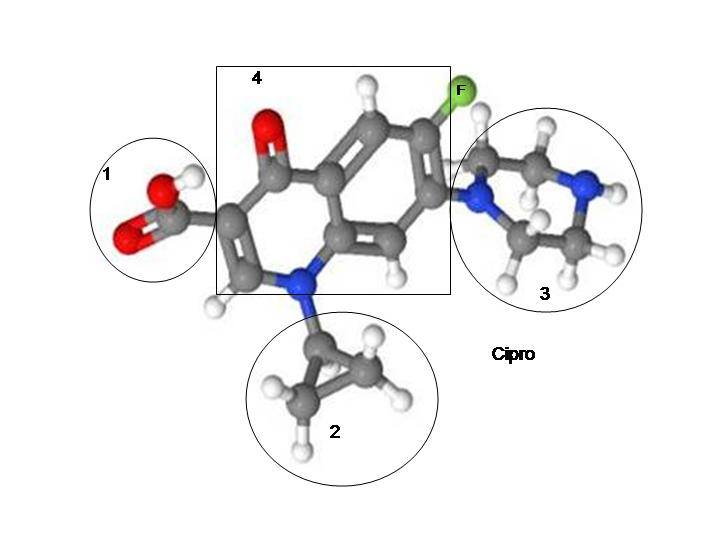
From the Cipro/ciprofloxacin warning label:
- Corticosteroid drugs increase the risk of tendon ruptures (in the black box warning).
- “Ciprofloxacin is an inhibitor of human cytochrome P450 1A2 (CYP1A2) mediated metabolism. Co-administration of ciprofloxacin with other drugs primarily metabolized by CYP1A2 results in increased plasma concentrations of these drugs and could lead to clinically significant adverse events of the co-administered drug.” Drugs metabolized by CYP1A2 include Alosetron/Lotronex, Caffeine, Clozapine/Clozaril, Flutamide/Eulexin, Frovatriptan/Frova, Melatonin, Mexiletine/Mexitil, Mirtazapine/Remeron, Olanzapine/Zyprexa, Ramelteon/Rozererm, Rasaglinie/Azilect, Robinirole/Requip, Tacrine/Cognex, Theophylline, Tizanidine/Zanaflex, Triamterene/Dyrenium, Zolmitriptan/Zomig (Source).
- “Concomitant administration with tizanidine is contraindicated”
- “Concomitant administration of ciprofloxacin with theophylline decreases the clearance of theophylline resulting in elevated serum theophylline levels and increased risk of a patient developing CNS or other adverse reactions.”
- “Ciprofloxacin also decreases caffeine clearance and inhibits the formation of paraxanthine after caffeine administration.”
- “Ciprofloxacin should be avoided in patients with known prolongation of the QT interval, risk factors for QT prolongation or torsade de pointes (for example, congenital long QT syndrome , uncorrected electrolyte imbalance, such as hypokalemia or hypomagnesemia and cardiac disease, such as heart failure, myocardial infarction, or bradycardia), and patients receiving Class IA antiarrhythmic agents (quinidine, procainamide), or Class III antiarrhythmic agents (amiodarone, sotalol), tricyclic antidepressants, macrolides, and antipsychotics.”
- “Altered serum levels of phenytoin (increased and decreased) have been reported in patients receiving concomitant ciprofloxacin.”
- “Hypoglycemia has been reported when ciprofloxacin and oral antidiabetic agents, mainly sulfonylureas (for example, glyburide, glimepiride), were co-administered, presumably by intensifying the action of the oral antidiabetic agent (see ADVERSE REACTIONS). The concomitant administration of ciprofloxacin with glyburide has, on rare occasions, resulted in severe hypoglycemia.”
- “Probenecid interferes with renal tubular secretion of ciprofloxacin and produces an increase in the level of ciprofloxacin in the serum.”
- “Renal tubular transport of methotrexate may be inhibited by concomitant administration of ciprofloxacin potentially leading to increased plasma levels of methotrexate.”
- “Metoclopramide significantly accelerates the absorption of oral ciprofloxacin resulting in shorter time to reach maximum plasma concentrations.”
- NSAIDs – “Non-steroidal anti-inflammatory drugs (but not acetyl salicylic acid) in combination of very high doses of quinolones have been shown to provoke convulsions in pre-clinical studies.”
There are many conditions that may (or may not) be related to fluoroquinolone toxicity that have “drugs to avoid” lists. Here are some of them:
- Myasthenia Gravis list of drugs to avoid
- Drugs that increase the QT interval
- G6PD Deficiency list of drugs to avoid
- Porphyria list of drugs to avoid
- Drugs that deplete magnesium
- Drugs that deplete iron
- Fluorinated Pharmaceuticals
- Drugs that contain carboxylic acid
There are a lot of questions about timing of drug administration that neither I, nor anyone else to my knowledge, know the answers to. It’s right there on the warning label that concurrent administration of ciprofloxacin and NSAIDs can induce convulsions (seizures), but does that mean that people who have taken ciprofloxacin in the past should avoid NSAIDs in the future? There is anecdotal evidence that NSAIDs should be avoided by floxies, but some people seem to handle them fine, and that’s valid anecdotal evidence too. When might it be safe for a floxie to take the drugs listed above? I don’t know the answer to that.
Another question that I don’t know the answer to is – Do adverse reactions to fluoroquinolones either uncover or cause another syndrome? Some of the possible syndromes that fluoroquinolone toxicity may or may not be related to are G6PD Deficiency and porphyria. Both G6PD Deficiency and porphyria can be brought on by adverse reactions to drugs. It’s possible that fluoroquinolone toxicity is related to these diseases, but I haven’t seen much evidence to support that assertion (so please just take it for what it’s worth).
I encourage everyone reading this to read the entire warning label for any drug you are prescribed, go over the potential benefits and risks with your doctor, and look up any drug you’re prescribed on www.askapatient.com and http://www.peoplespharmacy.com/. After that due diligence, I wish you luck with whatever decision you make. Know that fluoroquinolones are more dangerous than many, maybe most, drugs, and that sometimes pharmaceuticals are necessary, so try not to be too anxious about having to take one.
I hope this helps!









… [Trackback]
[…] Read More here to that Topic: floxiehope.com/pharmaceuticals-contraindicated-with-fqs/ […]
… [Trackback]
[…] Find More Info here on that Topic: floxiehope.com/pharmaceuticals-contraindicated-with-fqs/ […]
… [Trackback]
[…] Read More Information here on that Topic: floxiehope.com/pharmaceuticals-contraindicated-with-fqs/ […]
… [Trackback]
[…] Information on that Topic: floxiehope.com/pharmaceuticals-contraindicated-with-fqs/ […]
… [Trackback]
[…] Find More to that Topic: floxiehope.com/pharmaceuticals-contraindicated-with-fqs/ […]
… [Trackback]
[…] Find More on to that Topic: floxiehope.com/pharmaceuticals-contraindicated-with-fqs/ […]
… [Trackback]
[…] Here you will find 48580 more Info to that Topic: floxiehope.com/pharmaceuticals-contraindicated-with-fqs/ […]
… [Trackback]
[…] Information on that Topic: floxiehope.com/pharmaceuticals-contraindicated-with-fqs/ […]
… [Trackback]
[…] Information on that Topic: floxiehope.com/pharmaceuticals-contraindicated-with-fqs/ […]
… [Trackback]
[…] Here you can find 47052 more Information to that Topic: floxiehope.com/pharmaceuticals-contraindicated-with-fqs/ […]
… [Trackback]
[…] Find More Info here to that Topic: floxiehope.com/pharmaceuticals-contraindicated-with-fqs/ […]
… [Trackback]
[…] Read More on to that Topic: floxiehope.com/pharmaceuticals-contraindicated-with-fqs/ […]
… [Trackback]
[…] Information on that Topic: floxiehope.com/pharmaceuticals-contraindicated-with-fqs/ […]
… [Trackback]
[…] Information on that Topic: floxiehope.com/pharmaceuticals-contraindicated-with-fqs/ […]
… [Trackback]
[…] Info to that Topic: floxiehope.com/pharmaceuticals-contraindicated-with-fqs/ […]
… [Trackback]
[…] Read More Info here to that Topic: floxiehope.com/pharmaceuticals-contraindicated-with-fqs/ […]
… [Trackback]
[…] Info on that Topic: floxiehope.com/pharmaceuticals-contraindicated-with-fqs/ […]
… [Trackback]
[…] Here you will find 12411 more Info on that Topic: floxiehope.com/pharmaceuticals-contraindicated-with-fqs/ […]