After fluoroquinolone toxicity, many people have trouble handling NSAIDs. By “have trouble handling” I mean that NSAIDs lead to an explosion of fluoroquinolone toxicity related symptoms for many (but not all) people. I know that the last time I took a NSAID corresponded with the flox-bomb going off in my body – my hands and feet swelled and were painful, I had hives all over my body, my energy was gone, my tendons were weakened, my memory and concentration were shot, I had a massive amount of anxiety and many other symptoms. I intend to avoid NSAIDs for the rest of my life because of this, and other people’s similar experiences.
That’s nice anecdotal evidence, Lisa, but it’s anecdotal and therefore not very convincing.
From the warning label for Cipro/ciprofloxacin –
“NSAIDs – Non-steroidal anti-inflammatory drugs (but not acetyl salicylic acid) in combination of very high doses of quinolones have been shown to provoke convulsions in pre-clinical studies.”
Also, from Pharmacology Weekly, “convulsive seizures have been reported in patients taking fluoroquinolones, especially if they are also taking nonsteroidal antiinflammatory drugs (NSAIDs).”
Well, that sucks, but I’m not taking NSAIDs concurrently with fluoroquinolones and I haven’t had seizures. The question remains – Why shouldn’t I have NSAIDs after fluoroquinolone toxicity?
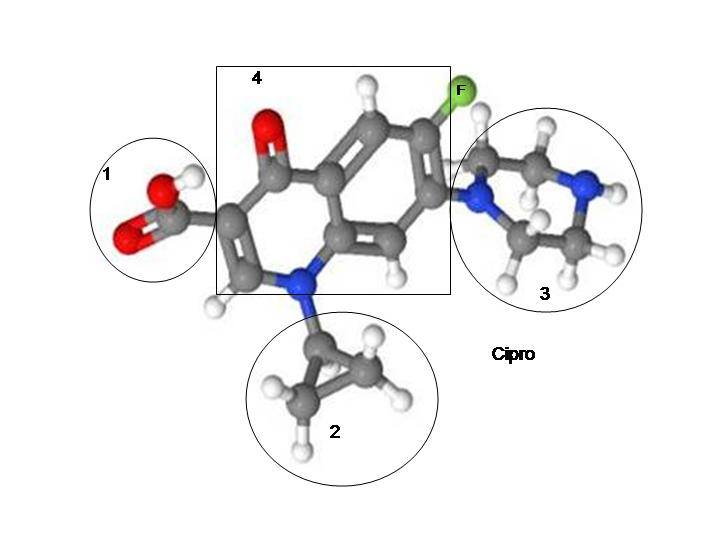
Nasty Carboxylic Acid Molecule
The answers, I think, come from the fact that both fluoroquinolones and NSAIDs have a carboxylic acid molecule in them.
When not metabolized properly, carboxylic acid molecule containing substances can form poisonous acyl-glucuronides and acyl-CoA thioesters. Poisonous metabolities. And, unfortunately, “When such metabolites react with critical proteins, cellular functionality may be disturbed or an immune response may be induced, eliciting adverse effects that in serious cases can be fatal” (from the article, Metabolic activation of carboxylic acids – all quotes in this post are from that article, unless otherwise specified).
Carboxylic acid molecules are found in various xenobiotics (a chemical or substance that is foreign to an organism or biological system), including fluoroquinolones and NSAIDs, as well as in biological systems “such as fatty acids, keto-acids, bile acids, messenger molecules and breakdown products from hormones and other endogenous molecules.” The existence of carboxylic acids in our natural environment and processes has led us to be able to metabolize carboxylic acid molecules well. Usually. Until we aren’t able to metabolize them well any longer. The conversion of carboxylic acid molecules into poisonous metabolites that react with proteins has to do with the following:
“It was also recognized early on that the isomers of acyl glucuronides (formed as a result of intramolecular acyl migration) can be equally or even more potent electrophilic species than the parent acyl glucuronide, and that these iso-glucuronides covalently bind to proteins via another mechanism [4]. Furthermore, acyl glucuronides are not only able to directly acylate cellular proteins, but they can also transacylate the cysteine thiol of glutathione (GSH), leading to drug-Sacyl- GSH, which in turn is a highly reactive species [5]. However, we still know very little about the overall toxicological significance of acyl glucuronides or their derivatives. A discussion about the causal role of acyl glucuronides in drug toxicity must not only consider the differential reactivity of the drug acyl glucuronides (e.g., type of substitution at the alpha carbon, half life [6-8]) but also the nature of the nucleophilic targets” from Editorial [Hot Topic:Acyl Glucuronides: Mechanistic Role in Drug Toxicity? (Guest Editor: Urs A. Boelsterli)] by Urs A. Boelsterli (213-214).
Got that? Don’t worry, most people don’t. Even the author of that quote, Urs A. Boelsterli, goes on to say that, “Like for other signaling paradigms, it seems that the complex balance between bioactivating and protective pathways may ultimately determine the outcome in vivo, rather than one single factor (reactivity of an acyl glucuronide) alone. Thus, the exact role of acyl glucuronides in drug safety assessment is simply not known and cannot be generalized.” Basically, it’s not known why carboxylic acid containing drugs sometimes turn into poisonous metabolites that form covalent adducts with critical protiens. They don’t always. But sometimes they do. And when they do, a whole load of bad health outcomes occur.
Removal of carboxylic acid containing drugs from the market
Many carboxylic acid containing drugs, including NSAIDs, have been removed from the market because of safety issues. “Many of the carboxylic acid containing drugs that have been associated with toxicity – idiosyncratic or otherwise – belong to the therapeutic class of NSAIDs.” And “Of 29 drugs withdrawn from the market in the UK, Spain or USA between 1974 and 1993, nine were carboxylic acid-containing drugs, making this compound class the most frequently involved in drug discontinuations in this period.”
Several fluoroquinolones have been removed from the market. Omniflox/temafloxacin, Raxar/grepafloxacin, Trovan/trovafloxacin, Zagam/sparfloxacin, and Tequin/gatifloxacin have all been taken off the market in the U.S.
Interactions between carboxylic acid containing drugs and mitochondria
Diclofenac is a NSAID that is still on the market despite its association with immune-mediated toxicity and hepatic failure. “studies have shown that diclofenac inhibits mitochondrial function, minimising ATP production and mitochondrial permeability transition [85,86] . Uncoupling of oxidative phosphorylation may be a class characteristic of NSAIDs and other carboxylic acid drugs; they act as proton ionophores.”
There is quite a bit of evidence that fluoroquinolones interfere with mitochondrial function “Bactericidal Antibiotics Induce Mitochondrial Dysfunction and Oxidative Damage in Mammalian Cells” and “Delayed cytotoxicity and cleavage of mitochondrial DNA in ciprofloxacin-treated mammalian cells” are two of my favorite articles. Also, the FDA admits that mitochondrial damage is the likely mechanism through which fluoroquinolones cause peripheral neuropathy.
Acyl-CoA thioester formation is one of the metabolic pathways through which carboxylic acid molecule containing substances can form “chemically reactive metabolites that are capable of participating in nucleophilic-type reactions leading to the formation of covalently bound protein adducts.” Acyl-CoA formation is “an integral part of mitochondrial energy metabolism.”
Delayed reactions and tolerance thresholds
A couple explanations for the delayed adverse reactions that people experience from fluoroquinolones come from the metabolites formed by the carboxylic acid molecules in FQs and NSAIDs, and also from their reaction with mitochondria. Urs Boelsterli notes that, “On the other hand, although glucuronidation of carboxylic acid-containing drugs may cause delayed toxicity due to reactive acyl glucuronide intermediates, this process may at the same time protect from the acute toxicity of the aglycone or its oxidative metabolite(s).” (Uhhhh…. Thanks for the delayed reaction that made this whole ordeal deniable for doctors? Well, it’s better than acute death, so there’s that.)
In “Mechanisms of Pathogenesis in Drug Hepatotoxicity Putting the Stress on Mitochondria” it is noted (by Urs Boelsterli and others) that:
“…damage to mitochondria often reflects successive chemical insults, such that no immediate cause for functional changes or pathological alterations can be established. There is indeed experimental evidence that prolonged injury to mitochondria, such as that which typifies oxidative injury to mitochondrial DNA or to components of the electron transport chain (ETC), has to cross a certain threshold (or a number of thresholds) before cell damage or cell death becomes manifest.”
To put this section in more simple terms, delayed reactions and tolerance thresholds are real and there are several hypotheses for why people experience delayed adverse reactions to fluoroquinolones, NSAIDs, and other carboxylic acid containing, mitochondria damaging drugs.
Staying in the Lipids
Another possible explanation for delayed reactions and relapses is that fluoroquinolones and NSAIDs stay in the body. I’ve always been skeptical about that possibility, but maybe they stay in the lipids. “For example, several studies have shown the ability of xenobiotic carboxylic acids to be incorporated into complex lipids (e.g., formation of ‘hybrid’ tri-acyl glycerols by ibuprofen or fenbufen [90-92] ), thus prolonging the time the drug stays in the body, or potentially causing adverse effects through inhibition of lipid-metabolizing enzymes etc. [93] . The toxicological effect of such hybrid lipids is not known at present.”
Fluoroquinolones thoroughly mess up lipids. The article “Comparison of the Effects of Subinhibitory Concentrations of Ciprofloxacin and Colistin on the Morphology of Cardiolipin Domains in Escherichia Coli Membranes” goes over how ciprofloxacin adversely affects cardiolipin, “an important component of the inner mitochondrial membrane, where it constitutes about 20% of the total lipid composition” (wiki). “Characterization of the Interactions between Fluoroquinolone Antibiotics and Lipids: a Multitechnique Approach” is also an informative article.
Something to note is that the tests for autoimmune diseases aren’t testing the activity of the immune system, as one might assume, they are testing for cellular damage antibodies. Antibodies to phospholipids are a category of tests for lupus, and the one of the tests in that category is that for a cardiolipin antibody.
Autoimmune Diseases and reactions
Some of the things said in “Metabolic activation of carboxylic acids” made me think that carboxylic acid containing drugs may be (causally) related to autoimmune diseases.
“high intra-cellular or plasma concentrations of acyl glucuronides may lead to the nonspecific formation of haptenated proteins that are able to invoke an immune response in susceptible individuals.”
“When such metabolites react with critical proteins, cellular functionality may be disturbed or an immune response may be induced, eliciting adverse effects that in serious cases can be fatal”
I’m honestly not sure whether or not the “immune response” noted is the same as an autoimmune disease.
It makes me wonder though – What is the relationship between carboxylic acid molecules and autoimmune diseases? The fact that both NSAIDs and hormones contain carboxylic acid molecules makes me wonder whether carboxylic acid metabolites are the reason that women have more problems with autoimmune diseases than men. (Women have a lovely monthly cycle of hormonal fluctuations that typically cause pain that is often treated with NSAIDs.)
The flox bomb went off in me 2 weeks after I finished my course of cipro, while I was taking NSAIDs (ibuprofen) because I was starting my period. Triple whammy. And it most definitely felt like my body was being attacked from the inside.
GABA issues
I honestly have no idea how GABA receptor issues relate to mitochondrial issues or carboxylic acid metabolism. I do know that messing with GABA-A receptors is another reason to avoid both fluoroquinolones and NSAIDs, and especially to avoid them together. From Pharmacology Weekly:
What role do NSAIDs have in the predisposition for developing seizures while also taking a fluoroquinolone antibiotic?
Interestingly, the presence of an NSAID or NSAID metabolite can significantly augment this effect and result in an even greater inhibition of GABA-A receptor activity. It is, however, important to note that majority of this effect is related to an NSAID that is only available outside of the United States called fenbufen (Afiancen®, Bifene®, Cincopal®, Cinopal®, Lederfen®, Reugast®).9-11,14 It appears that the metabolite of fenbufen, 4-biphenylacetic acid (BPAA), augments the ability of the fluoroquinolone to inhibit GABA binding to the GABA-A receptor.9-11,14 It is important to note that BPPA itself does not inhibit GABA binding to the GABA-A receptor, but rather when BPAA and the fluoroquinolone come in close proximity they interact in such a way that it results in the ability of the fluoroquinolone antibiotic to inhibit GABA binding to a greater degree than by itself. It is possible that the interaction between a fluoroquinolone antibiotic and BPAA causes some other biologic effect that influences the activity of the GABA-A receptor. In fact, there is some evidence that some fluoroquinolones (mainly enoxacin and norfloxacin) can increase the activity of nuclear activator protein 1 (AP-1) DNA- and cyclic AMP responsive elements (CRE)-binding activities in both the hippocampus and cerebral cortex.14 It has been suggested that increased activity of AP-1 mediated gene expression is important for activity-dependent plasticity in these regions of the brain and thus contribute to the increased risk for seizures.14 Even though fenbufen has been the main NSAID implicated in this adverse drug reaction, other NSAIDs such as indomethacin, ketoprofen, naproxen, ibuprofen have also been shown to augment fluoroquinolone induced GABA-A receptor inhibition in animal studies.9
While the data most strongly implicate certain fluoroquinolone antibiotics and NSAIDs, CNS side effects and seizures have been reported with many of the fluoroquinolones, including the ones currently on the market.1-5 This is the reason that the product package inserts for the fluoroquinolone antibiotics not only list the above as potential side effects, but also describe the drug interaction with NSAIDs.1-5 As such, until further evidence suggests otherwise, it would be prudent, especially from a medical legal perspective, for healthcare providers to avoid the use of fluoroquinolones with or without NSAIDs in patients who are at greater risk for seizures (e.g., history of epilepsy, severe cerebral arteriosclerosis) or those with a lower seizure threshold (e.g., patients on medications known to do this, renal dysfunction).
Heart Disease
Even if one has never taken a fluoroquinolone, NSAIDs should be used with caution. The number of NSAIDs removed from the market because they were too dangerous is high. Vioxx, ibufenac, benoxaprofen have all been removed from the market because of severe toxicity issues. Vioxx is thought to have directly caused hundreds of thousands of heart attacks.
The Reuters article, “High doses of common painkillers increase heart attack risks” notes that, “Long-term high-dose use of painkillers such as ibuprofen or diclofenac is ‘equally hazardous’ in terms of heart attack risk as use of the drug Vioxx, which was withdrawn due to its potential dangers, researchers said on Thursday.”
Concluding thoughts
Before I got floxed, I would pop ibuprofen like it was candy. I would take it to ease menstrual cramps, whenever I felt even a little bit achy, and even to help me sleep. I never had any sort of adverse reaction to it. I thought of it as “vitamin I.”
It was only after my second exposure to cipro that I could no longer handle ibuprofen. As I mentioned, the explosion that occurred in my body after taking cipro corresponded with taking ibuprofen for menstrual cramps. I have not taken an NSAID since and I intend to avoid them, along with every other carboxylic acid containing drug, indefinitely.
Maybe my frequent use of ibuprofen set me up for getting floxed later.
Maybe the horrible reaction that I had to the triple whammy of carboxylic acid molecule containing substances – cipro, ibuprofen and hormones – saved me from future long-term consequences of regular NSAID use. I don’t know. I do know that they’re nasty drugs. Shoot, NSAIDs can cause Stevens-Johnson Syndrome – aka, the worst thing ever, so I’m glad I stay away from them now.
Got it, no NSAIDs. Problem – I’M STILL IN PAIN! Any suggestions?
A paragraph at the end of an already-too-long post isn’t the place to fully address this, but I will acknowledge that the lack of safe painkillers is a serious problem. Here are some options that I have heard good things about (I’m not a doctor, this isn’t medical advice, yadayada) –
- Tumeric
- Tart Cherry Juice
- Vitamin D3
- Cannabis / Marijuana
- Opiates (a crappy option in many ways)
- Acetaminophen / Tylenol (it’s hard on your liver, but it’s not a NSAID)
Here’s an article from Dr. Mercola that lists some additional alternative to pharmaceutical painkillers – http://articles.mercola.com/sites/articles/archive/2014/10/02/narcotic-overdose-deaths.aspx










I find this very interesting because for the two weeks I was taking the antibiotic (post op) I was also prescribed to take 800mg of ibuprofen every 6 hours. This was in addition to my Rx pain pills. AND after I had general anesthesia for 4 hours. I feel this all created the perfect storm. I am thinking that one of those things ALONE may not have caused such problems. But altogether…man…
Oh that’s fine. Yes I did – however I kept my ovaries. Haven’t noticed too much difference in hormonal issues. Still get PMS and all that (grrrr).
If carboxylic acid is found in bile acids, does this mean that digestive enzymes made from bile are a no no for floxed people?
Sent from my iPhone
Cannabis never worked for me. I tried it for pain years ago. I remember hearing of some research that it can damage DNA. Who needs that on top of all the other damage? My peripheral neuropathy didn’t start until 6 months out when my tendons were starting to improve. Now 16 months out they are worse again. It is very depressing but I think if you just live one day at a time you will make it through. Lisa thank you for all your research. You do give people hope. I don’t know what I would have done without this website.
In support of ORGANIC Foods: Frontline also reports that meat may be a source of potentially lethal infections—not simply because you’re eating antibiotics and therefore building resistance, but because the meat is tainted with drug-resistant bacteria that can cause disease if the meat is improperly handled or undercooked.
One example given is drug-resistant urinary infections, which are on the rise. If the antibiotics fail to wipe out the bacteria, the infection can progress to your kidneys, which allows the bacteria access to your blood. The result is sepsis, which kills 40,000 Americans each year.
Using state of the art genome sequencing, researchers were able to compare E.coli samples found on supermarket meat with E.coli samples collected from patients with drug-resistant urinary tract infections. In this way, they were able to genetically link more than 100 urinary tract infections to tainted supermarket meat products.
Lisa, look at this compound
2-hydroxypropane-1,2,3-tricarboxylic acid
1-cyclopropyl-6-fluoro-4-oxo-7-(piperazin-1-yl)-quinoline-3-carboxylic acid
First is Citric Acid, second is Cipro.
Since the Citric Acid Cycle (Krebs) is vitally important to oxidative phosphorylation, I wonder if somehow FQ’s disrupt this cycle in some way?
http://en.wikipedia.org/wiki/Citric_acid_cycle
I also wonder then if some compound like citric acid could cause more issues. I know of a few floxies that say they get worse after ingesting lemon juice, etc. Just some thoughts.
http://en.wikipedia.org/wiki/Carboxylic_acid It’s in everything…. 🙂
For reference, here are some interesting posts about the dangers of NSAIDs:
From Chandler Marrs on Hormones Matter – http://www.hormonesmatter.com/nsaids-painkillers-arrhythmia/
From Dr. John M on his (very good) blog – http://www.drjohnm.org/2014/02/nsaids-yet-another-dubious-health-product-at-cvs/
Hi Lisa. So is regular Aspirin ok then? (acetylsalicylic acid)
Hello Lisa ! I am glad I ran across this post somewhat by accident today. I had thought that maybe Diclofenac was a bit less evil, rather than more, with NSAIDS. It was kind of described that way to me by my former Primary Doctor who was trying to manage my issues of low back injury with sciatica, excessive migraine and toxic reaction to Gadolinium dye. They are kind of Nazis here about giving anyone opiates or controlled substance for pain, which I kind of understand and appreciate, but it seems like it maybe would have been a safer temporary option for my worst times if there was no addiction or abuse. I took a pretty fair amount of it, at their insistence and I am glad that I haven’t been a patient there for about 4 years because they didn’t manage anything very well. I also was not sure if Acetaminophen is considered NSAID or not, though I do know it is toxic to liver and with most opiates, you’re still getting dosed with Acetaminophen, like it or not. I am 22 months since the Cipro. Low back pain and complete loss of feeling in left leg has made me desperate for some sort of relief. As much as I didn’t want to do it. I tried the Prednisone about 3 days and Naproxen for just one day. No and no, still reacting badly. Thanks for your time and efforts concerning FQ issues. I hope you are doing well !
People often ask what alternatives to NSAIDs are. There is a list of alternative painkillers in this post – http://www.greenmedinfo.com/blog/ibuprofen-kills-more-pain-so-what-alternatives
NSAIDs and Cortisone seems to cause Cipro damage flares for people.
The GUT connection – Autoimmune Diseases and reactions
LEAKY GUT is one of THE most common ROOT causes of Autoimmune Diseases, and NSAIDS can cause a Leaky Gut.
http://www.drperlmutter.com/nsaids-gut-inflammation/?hvid=1ZQDcg
“It is now recognized that certain medications may lead to increased bowel permeability as well. There has been a lot of attention given to the role of nonsteroidal anti-inflammatory drugs (NSAIDs) in terms of damaging the gut lining and leading to inflammation, the very problem for which these drugs have been designed to help!
New research demonstrates in the laboratory animal that exposure to NSAIDs not only compromises the barrier function of the lining, but in addition, and probably because of the effects upon the gut lining, this class of medications, at least in the laboratory animal, induce gluten sensitivity.”
NSAID Enteropathy – Damage to the Small Intestine has an official name as well it is SO common
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3237301/
“Non-steroidal anti-inflammatory drug (NSAID)-induced small bowel injury is a topic that deserves attention since the advent of capsule endoscopy and balloon enteroscopy. NSAID enteropathy is common, the pathogenesis of small intestine injury by NSAIDs is complex and different from that of the upper gastrointestinal tract.”
Biome damage http://www.ncbi.nlm.nih.gov/pubmed/16498262
Microbial flora in NSAID-induced intestinal damage
Upper gastrointestinal (GI) complications are well-recognized adverse events associated with non-steroidal anti-inflammatory drug (NSAID) use. However, NSAID-induced damage to the distal GI tract is also common and more frequent than previously recognized. These untoward effects include increased mucosal permeability, mucosal inflammation, anemia and occult blood loss, malabsorption, protein loss, ileal dysfunction, diarrhea, mucosal ulceration, strictures due to diaphragm disease as well as active bleeding and perforation. Studies with selective COX-2 inhibitors have shown that, in the short term, these agents do not increase mucosal permeability and display a reduced by 50% incidence of serious lower GI side effects compared to traditional NSAIDs. However, the long-term use of this therapeutic strategy is limited by the increased risk of serious cardiovascular events, especially in patients with multiple risk factors. Several studies have suggested that intraluminal bacteria play a significant role in the pathogenesis of small-bowel damage induced by NSAIDs and that enterobacterial translocation into the mucosa represents the first step that sets in motion a series of events leading to gross lesion formation. Experimental and clinical investigations indicate that in the short term, antibacterial agents either reduce or abolish NSAID enteropathy. However, potential adverse effects of systemic antimicrobials and the possible occurrence of drug resistance have so far precluded this interesting approach. The availability of poorly absorbed and effective antibiotics, like rifaximin, may represent an attractive alternative to prevent or limit NSAID-associated intestinal damage.
Has anyone tried topical Magnesium Oil. For me, after daily applications for 2 months much of my pain went away, and strength returned. That is until I took 2 ibuprofen, and have a bit of a setback.
The above article about NSIDS and their cellular damage, mentioned Vioxx, a Cox II inhibitor developed for people who, for various reasons, were unable to take the stronger NSAIDS. The only Cox II inhibitor left on the market is Celebrex. Because I developed strictures and erosions in my distal small bowel ,total 16 inches (looked like link-sausage)which required resection at 2 places, January, 2016, thought to be from 40 years on Voltaren.
Now my PCP and GI docs are against me taking even Celebrex on a long term basis. Without it, my quality of life drops to -15. Seriously, I can’t move. I have taken the non-shell fish glucosamine, chondroitin, MSM and the newly on the market Curcumin BCM-95. Plus a host of other antioxidants. The jury is still out on them, but, they are the most recommended.
Some of the literature indicated some “floxed” patients responded to glutathione IV. I found an integrative Medicine MD and received 3 slowly increased doses, but ended up in the hospital from at least partially the doctor’s detoxification substances, and through the process I learned that he had been sanctioned 3 times by his state’s Medical Board for several omissions. Even though I fell short of the desired numbered of doses, I feel it did benefit me to some extent. I learned not to trust a well developed website, but to use the several sites that critic doctors and their practice history.
Hi,
the text above and coments are really helpful.
My problem is, that i have arthritis (Reactive probably) and i need to take something. My doctor give me a Aclexa (Celecoxibum) which is NSAID, so i’m really scary to take it.
Do you have any ideas what i should take instead of Aclexa?
My Dr. keeps wanting me to take a baby aspirin a day as a blood thinner. Though the warning says it is ok, Aspirin does have a carboxylic acid group so I am afraid to take it. Any thoughts on this from anyone? Has anyone taken aspirin and been ok? Does anyone know what else to take as a natural blood thinner? I am 2 years out from floxing.
3,5 years out of floxing I took one Diclofenac (NSAID) and the hell broke out again, much worse then the first time (and this was really worse, too). I was out of work for nearly three month. Tremors, weakness, panic attacks, visual problems, eye pain, temperature issues, brain fog, depersonalization, insomnia, hair is falling out and peripheral neuropathy. Still suffering and hope for healing again…