After fluoroquinolone toxicity, many people have trouble handling NSAIDs. By “have trouble handling” I mean that NSAIDs lead to an explosion of fluoroquinolone toxicity related symptoms for many (but not all) people. I know that the last time I took a NSAID corresponded with the flox-bomb going off in my body – my hands and feet swelled and were painful, I had hives all over my body, my energy was gone, my tendons were weakened, my memory and concentration were shot, I had a massive amount of anxiety and many other symptoms. I intend to avoid NSAIDs for the rest of my life because of this, and other people’s similar experiences.
That’s nice anecdotal evidence, Lisa, but it’s anecdotal and therefore not very convincing.
From the warning label for Cipro/ciprofloxacin –
“NSAIDs – Non-steroidal anti-inflammatory drugs (but not acetyl salicylic acid) in combination of very high doses of quinolones have been shown to provoke convulsions in pre-clinical studies.”
Also, from Pharmacology Weekly, “convulsive seizures have been reported in patients taking fluoroquinolones, especially if they are also taking nonsteroidal antiinflammatory drugs (NSAIDs).”
Well, that sucks, but I’m not taking NSAIDs concurrently with fluoroquinolones and I haven’t had seizures. The question remains – Why shouldn’t I have NSAIDs after fluoroquinolone toxicity?
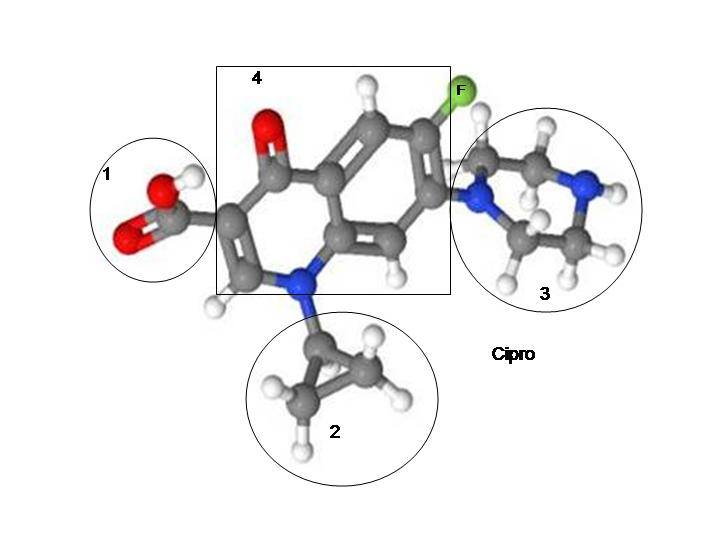
Nasty Carboxylic Acid Molecule
The answers, I think, come from the fact that both fluoroquinolones and NSAIDs have a carboxylic acid molecule in them.
When not metabolized properly, carboxylic acid molecule containing substances can form poisonous acyl-glucuronides and acyl-CoA thioesters. Poisonous metabolities. And, unfortunately, “When such metabolites react with critical proteins, cellular functionality may be disturbed or an immune response may be induced, eliciting adverse effects that in serious cases can be fatal” (from the article, Metabolic activation of carboxylic acids – all quotes in this post are from that article, unless otherwise specified).
Carboxylic acid molecules are found in various xenobiotics (a chemical or substance that is foreign to an organism or biological system), including fluoroquinolones and NSAIDs, as well as in biological systems “such as fatty acids, keto-acids, bile acids, messenger molecules and breakdown products from hormones and other endogenous molecules.” The existence of carboxylic acids in our natural environment and processes has led us to be able to metabolize carboxylic acid molecules well. Usually. Until we aren’t able to metabolize them well any longer. The conversion of carboxylic acid molecules into poisonous metabolites that react with proteins has to do with the following:
“It was also recognized early on that the isomers of acyl glucuronides (formed as a result of intramolecular acyl migration) can be equally or even more potent electrophilic species than the parent acyl glucuronide, and that these iso-glucuronides covalently bind to proteins via another mechanism [4]. Furthermore, acyl glucuronides are not only able to directly acylate cellular proteins, but they can also transacylate the cysteine thiol of glutathione (GSH), leading to drug-Sacyl- GSH, which in turn is a highly reactive species [5]. However, we still know very little about the overall toxicological significance of acyl glucuronides or their derivatives. A discussion about the causal role of acyl glucuronides in drug toxicity must not only consider the differential reactivity of the drug acyl glucuronides (e.g., type of substitution at the alpha carbon, half life [6-8]) but also the nature of the nucleophilic targets” from Editorial [Hot Topic:Acyl Glucuronides: Mechanistic Role in Drug Toxicity? (Guest Editor: Urs A. Boelsterli)] by Urs A. Boelsterli (213-214).
Got that? Don’t worry, most people don’t. Even the author of that quote, Urs A. Boelsterli, goes on to say that, “Like for other signaling paradigms, it seems that the complex balance between bioactivating and protective pathways may ultimately determine the outcome in vivo, rather than one single factor (reactivity of an acyl glucuronide) alone. Thus, the exact role of acyl glucuronides in drug safety assessment is simply not known and cannot be generalized.” Basically, it’s not known why carboxylic acid containing drugs sometimes turn into poisonous metabolites that form covalent adducts with critical protiens. They don’t always. But sometimes they do. And when they do, a whole load of bad health outcomes occur.
Removal of carboxylic acid containing drugs from the market
Many carboxylic acid containing drugs, including NSAIDs, have been removed from the market because of safety issues. “Many of the carboxylic acid containing drugs that have been associated with toxicity – idiosyncratic or otherwise – belong to the therapeutic class of NSAIDs.” And “Of 29 drugs withdrawn from the market in the UK, Spain or USA between 1974 and 1993, nine were carboxylic acid-containing drugs, making this compound class the most frequently involved in drug discontinuations in this period.”
Several fluoroquinolones have been removed from the market. Omniflox/temafloxacin, Raxar/grepafloxacin, Trovan/trovafloxacin, Zagam/sparfloxacin, and Tequin/gatifloxacin have all been taken off the market in the U.S.
Interactions between carboxylic acid containing drugs and mitochondria
Diclofenac is a NSAID that is still on the market despite its association with immune-mediated toxicity and hepatic failure. “studies have shown that diclofenac inhibits mitochondrial function, minimising ATP production and mitochondrial permeability transition [85,86] . Uncoupling of oxidative phosphorylation may be a class characteristic of NSAIDs and other carboxylic acid drugs; they act as proton ionophores.”
There is quite a bit of evidence that fluoroquinolones interfere with mitochondrial function “Bactericidal Antibiotics Induce Mitochondrial Dysfunction and Oxidative Damage in Mammalian Cells” and “Delayed cytotoxicity and cleavage of mitochondrial DNA in ciprofloxacin-treated mammalian cells” are two of my favorite articles. Also, the FDA admits that mitochondrial damage is the likely mechanism through which fluoroquinolones cause peripheral neuropathy.
Acyl-CoA thioester formation is one of the metabolic pathways through which carboxylic acid molecule containing substances can form “chemically reactive metabolites that are capable of participating in nucleophilic-type reactions leading to the formation of covalently bound protein adducts.” Acyl-CoA formation is “an integral part of mitochondrial energy metabolism.”
Delayed reactions and tolerance thresholds
A couple explanations for the delayed adverse reactions that people experience from fluoroquinolones come from the metabolites formed by the carboxylic acid molecules in FQs and NSAIDs, and also from their reaction with mitochondria. Urs Boelsterli notes that, “On the other hand, although glucuronidation of carboxylic acid-containing drugs may cause delayed toxicity due to reactive acyl glucuronide intermediates, this process may at the same time protect from the acute toxicity of the aglycone or its oxidative metabolite(s).” (Uhhhh…. Thanks for the delayed reaction that made this whole ordeal deniable for doctors? Well, it’s better than acute death, so there’s that.)
In “Mechanisms of Pathogenesis in Drug Hepatotoxicity Putting the Stress on Mitochondria” it is noted (by Urs Boelsterli and others) that:
“…damage to mitochondria often reflects successive chemical insults, such that no immediate cause for functional changes or pathological alterations can be established. There is indeed experimental evidence that prolonged injury to mitochondria, such as that which typifies oxidative injury to mitochondrial DNA or to components of the electron transport chain (ETC), has to cross a certain threshold (or a number of thresholds) before cell damage or cell death becomes manifest.”
To put this section in more simple terms, delayed reactions and tolerance thresholds are real and there are several hypotheses for why people experience delayed adverse reactions to fluoroquinolones, NSAIDs, and other carboxylic acid containing, mitochondria damaging drugs.
Staying in the Lipids
Another possible explanation for delayed reactions and relapses is that fluoroquinolones and NSAIDs stay in the body. I’ve always been skeptical about that possibility, but maybe they stay in the lipids. “For example, several studies have shown the ability of xenobiotic carboxylic acids to be incorporated into complex lipids (e.g., formation of ‘hybrid’ tri-acyl glycerols by ibuprofen or fenbufen [90-92] ), thus prolonging the time the drug stays in the body, or potentially causing adverse effects through inhibition of lipid-metabolizing enzymes etc. [93] . The toxicological effect of such hybrid lipids is not known at present.”
Fluoroquinolones thoroughly mess up lipids. The article “Comparison of the Effects of Subinhibitory Concentrations of Ciprofloxacin and Colistin on the Morphology of Cardiolipin Domains in Escherichia Coli Membranes” goes over how ciprofloxacin adversely affects cardiolipin, “an important component of the inner mitochondrial membrane, where it constitutes about 20% of the total lipid composition” (wiki). “Characterization of the Interactions between Fluoroquinolone Antibiotics and Lipids: a Multitechnique Approach” is also an informative article.
Something to note is that the tests for autoimmune diseases aren’t testing the activity of the immune system, as one might assume, they are testing for cellular damage antibodies. Antibodies to phospholipids are a category of tests for lupus, and the one of the tests in that category is that for a cardiolipin antibody.
Autoimmune Diseases and reactions
Some of the things said in “Metabolic activation of carboxylic acids” made me think that carboxylic acid containing drugs may be (causally) related to autoimmune diseases.
“high intra-cellular or plasma concentrations of acyl glucuronides may lead to the nonspecific formation of haptenated proteins that are able to invoke an immune response in susceptible individuals.”
“When such metabolites react with critical proteins, cellular functionality may be disturbed or an immune response may be induced, eliciting adverse effects that in serious cases can be fatal”
I’m honestly not sure whether or not the “immune response” noted is the same as an autoimmune disease.
It makes me wonder though – What is the relationship between carboxylic acid molecules and autoimmune diseases? The fact that both NSAIDs and hormones contain carboxylic acid molecules makes me wonder whether carboxylic acid metabolites are the reason that women have more problems with autoimmune diseases than men. (Women have a lovely monthly cycle of hormonal fluctuations that typically cause pain that is often treated with NSAIDs.)
The flox bomb went off in me 2 weeks after I finished my course of cipro, while I was taking NSAIDs (ibuprofen) because I was starting my period. Triple whammy. And it most definitely felt like my body was being attacked from the inside.
GABA issues
I honestly have no idea how GABA receptor issues relate to mitochondrial issues or carboxylic acid metabolism. I do know that messing with GABA-A receptors is another reason to avoid both fluoroquinolones and NSAIDs, and especially to avoid them together. From Pharmacology Weekly:
What role do NSAIDs have in the predisposition for developing seizures while also taking a fluoroquinolone antibiotic?
Interestingly, the presence of an NSAID or NSAID metabolite can significantly augment this effect and result in an even greater inhibition of GABA-A receptor activity. It is, however, important to note that majority of this effect is related to an NSAID that is only available outside of the United States called fenbufen (Afiancen®, Bifene®, Cincopal®, Cinopal®, Lederfen®, Reugast®).9-11,14 It appears that the metabolite of fenbufen, 4-biphenylacetic acid (BPAA), augments the ability of the fluoroquinolone to inhibit GABA binding to the GABA-A receptor.9-11,14 It is important to note that BPPA itself does not inhibit GABA binding to the GABA-A receptor, but rather when BPAA and the fluoroquinolone come in close proximity they interact in such a way that it results in the ability of the fluoroquinolone antibiotic to inhibit GABA binding to a greater degree than by itself. It is possible that the interaction between a fluoroquinolone antibiotic and BPAA causes some other biologic effect that influences the activity of the GABA-A receptor. In fact, there is some evidence that some fluoroquinolones (mainly enoxacin and norfloxacin) can increase the activity of nuclear activator protein 1 (AP-1) DNA- and cyclic AMP responsive elements (CRE)-binding activities in both the hippocampus and cerebral cortex.14 It has been suggested that increased activity of AP-1 mediated gene expression is important for activity-dependent plasticity in these regions of the brain and thus contribute to the increased risk for seizures.14 Even though fenbufen has been the main NSAID implicated in this adverse drug reaction, other NSAIDs such as indomethacin, ketoprofen, naproxen, ibuprofen have also been shown to augment fluoroquinolone induced GABA-A receptor inhibition in animal studies.9
While the data most strongly implicate certain fluoroquinolone antibiotics and NSAIDs, CNS side effects and seizures have been reported with many of the fluoroquinolones, including the ones currently on the market.1-5 This is the reason that the product package inserts for the fluoroquinolone antibiotics not only list the above as potential side effects, but also describe the drug interaction with NSAIDs.1-5 As such, until further evidence suggests otherwise, it would be prudent, especially from a medical legal perspective, for healthcare providers to avoid the use of fluoroquinolones with or without NSAIDs in patients who are at greater risk for seizures (e.g., history of epilepsy, severe cerebral arteriosclerosis) or those with a lower seizure threshold (e.g., patients on medications known to do this, renal dysfunction).
Heart Disease
Even if one has never taken a fluoroquinolone, NSAIDs should be used with caution. The number of NSAIDs removed from the market because they were too dangerous is high. Vioxx, ibufenac, benoxaprofen have all been removed from the market because of severe toxicity issues. Vioxx is thought to have directly caused hundreds of thousands of heart attacks.
The Reuters article, “High doses of common painkillers increase heart attack risks” notes that, “Long-term high-dose use of painkillers such as ibuprofen or diclofenac is ‘equally hazardous’ in terms of heart attack risk as use of the drug Vioxx, which was withdrawn due to its potential dangers, researchers said on Thursday.”
Concluding thoughts
Before I got floxed, I would pop ibuprofen like it was candy. I would take it to ease menstrual cramps, whenever I felt even a little bit achy, and even to help me sleep. I never had any sort of adverse reaction to it. I thought of it as “vitamin I.”
It was only after my second exposure to cipro that I could no longer handle ibuprofen. As I mentioned, the explosion that occurred in my body after taking cipro corresponded with taking ibuprofen for menstrual cramps. I have not taken an NSAID since and I intend to avoid them, along with every other carboxylic acid containing drug, indefinitely.
Maybe my frequent use of ibuprofen set me up for getting floxed later.
Maybe the horrible reaction that I had to the triple whammy of carboxylic acid molecule containing substances – cipro, ibuprofen and hormones – saved me from future long-term consequences of regular NSAID use. I don’t know. I do know that they’re nasty drugs. Shoot, NSAIDs can cause Stevens-Johnson Syndrome – aka, the worst thing ever, so I’m glad I stay away from them now.
Got it, no NSAIDs. Problem – I’M STILL IN PAIN! Any suggestions?
A paragraph at the end of an already-too-long post isn’t the place to fully address this, but I will acknowledge that the lack of safe painkillers is a serious problem. Here are some options that I have heard good things about (I’m not a doctor, this isn’t medical advice, yadayada) –
- Tumeric
- Tart Cherry Juice
- Vitamin D3
- Cannabis / Marijuana
- Opiates (a crappy option in many ways)
- Acetaminophen / Tylenol (it’s hard on your liver, but it’s not a NSAID)
Here’s an article from Dr. Mercola that lists some additional alternative to pharmaceutical painkillers – http://articles.mercola.com/sites/articles/archive/2014/10/02/narcotic-overdose-deaths.aspx











“NSAIDs – Non-steroidal anti-inflammatory drugs (but not acetyl salicylic acid) in combination of very high doses of quinolones have been shown to provoke convulsions in pre-clinical studies.”
So, in your experience, is Aspirin safe to take?
I’m suffering from a noninfectious urethritis, and taking acetaminophen, wich I’ve read here, is safer, would be useless in my case. Any suggestion ?
Thanks.
Has anyone tried oral steroids for inflammation, after being floxed? I know you shouldn’t take steroids while taking Cipro, but what about long after? My experience with Cipro occurred 3 months ago. I have recovered from all symptoms, except my under eye muscle is still swollen. I want to take steroids to chase the swelling out, but I am afraid of interactions.
i saw that pepto bismol is also an nsaid. anyone have experience with it?
… [Trackback]
[…] Read More here to that Topic: floxiehope.com/why-nsaids-suck-for-floxies-and-probably-everyone-else-too/ […]
… [Trackback]
[…] Read More here to that Topic: floxiehope.com/why-nsaids-suck-for-floxies-and-probably-everyone-else-too/ […]
… [Trackback]
[…] Read More Info here on that Topic: floxiehope.com/why-nsaids-suck-for-floxies-and-probably-everyone-else-too/ […]
… [Trackback]
[…] Read More Information here to that Topic: floxiehope.com/why-nsaids-suck-for-floxies-and-probably-everyone-else-too/ […]
… [Trackback]
[…] Here you will find 66158 additional Information to that Topic: floxiehope.com/why-nsaids-suck-for-floxies-and-probably-everyone-else-too/ […]
… [Trackback]
[…] Read More on to that Topic: floxiehope.com/why-nsaids-suck-for-floxies-and-probably-everyone-else-too/ […]
… [Trackback]
[…] Find More on that Topic: floxiehope.com/why-nsaids-suck-for-floxies-and-probably-everyone-else-too/ […]
… [Trackback]
[…] Find More here to that Topic: floxiehope.com/why-nsaids-suck-for-floxies-and-probably-everyone-else-too/ […]
… [Trackback]
[…] Read More to that Topic: floxiehope.com/why-nsaids-suck-for-floxies-and-probably-everyone-else-too/ […]
… [Trackback]
[…] Read More to that Topic: floxiehope.com/why-nsaids-suck-for-floxies-and-probably-everyone-else-too/ […]
… [Trackback]
[…] Here you will find 48405 additional Information on that Topic: floxiehope.com/why-nsaids-suck-for-floxies-and-probably-everyone-else-too/ […]
… [Trackback]
[…] Find More on to that Topic: floxiehope.com/why-nsaids-suck-for-floxies-and-probably-everyone-else-too/ […]
… [Trackback]
[…] There you will find 67383 additional Information on that Topic: floxiehope.com/why-nsaids-suck-for-floxies-and-probably-everyone-else-too/ […]
… [Trackback]
[…] Info to that Topic: floxiehope.com/why-nsaids-suck-for-floxies-and-probably-everyone-else-too/ […]
… [Trackback]
[…] Read More Information here to that Topic: floxiehope.com/why-nsaids-suck-for-floxies-and-probably-everyone-else-too/ […]
… [Trackback]
[…] Here you will find 24709 more Information on that Topic: floxiehope.com/why-nsaids-suck-for-floxies-and-probably-everyone-else-too/ […]
… [Trackback]
[…] Read More to that Topic: floxiehope.com/why-nsaids-suck-for-floxies-and-probably-everyone-else-too/ […]